Introduction
Parkinson’s disease is caused by a drop in dopamine levels resulting from nerve cell damage. People with Parkinson’s disease experience unintended movements such as shaking and difficulty with balance and coordination. Parkinson’s disease is a degenerative condition of the brain associated with motor symptoms and non-motor complications (WHO, 2022). The severity of the disease progresses with age and causes movement problems for older people. Different aspects of Parkinson’s disease (PD) are explored, providing valuable insights that enhance readers’ understanding of how to manage the condition.
Description, Causes, and Symptoms of Parkinson’s Disease
Description and Definition
PD is associated with clinical features such as rest tremors, rigidity, and bradykinesia. Parkinson’s disease is associated with motor symptoms, such as slow movement, and non-motor symptoms, such as sleep disorders (WHO, 2022). According to WHO (2022), “PD resulted in 5.8 million disability-adjusted life years, an increase of 81% since 2000, causing 329,000 deaths, an increase of over 100% since 2000” (para, 5).
Tremors are involuntary, rhythmic muscle contractions leading to shaking movements and are associated with stress, physical exhaustion, or low blood sugar that affect part of the brain that controls movement (NINDS, 202I). Rigidity occurs when muscles involuntarily tighten, while bradykinesia refers to slow movement. All these clinical features combined result in Parkinson’s disease in the affected person.
Causes
Parkinson’s disease occurs when nerve cells in the basal ganglia, an area of the brain that controls movement, become impaired or die. The neurons’ death or impairment reduces dopamine production, which causes movement problems associated with the disease. Working with heavy metals and detergents triggers Parkinson’s disease (Hopkins, 2022). Such environmental factors increase the risk of getting Parkinson’s disease. Parkinson’s disease can be hereditary, which becomes evident when some genetic factors combine with environmental factors, such as exposure to toxins. Age is crucial, as the disease mainly begins at sixty and affects more men than women.
Symptoms
Many signs and symptoms are associated with Parkinson’s disease, making it easy to discover at early stages. Some movement-related symptoms are tremors in hands, arms, legs, and jaws, muscle stiffness, loss of automatic movements such as blinking, slow mobility, and impaired balance. Non-motor symptoms like depression, constipation, skin problems, and difficulties in sleeping are evident when a person has Parkinson’s disease. The symptoms occur gradually, and the signs are mild at first, but they escalate as the disease progresses. These symptoms may seem to occur in other normally aging people, making it necessary to consult a physician when someone experiences them.
Surveillance and Reporting
A study on patients with idiopathic Parkinson’s disease showed that a disease monitoring system is feasible for a diverse Parkinson’s disease population. Patients had wearable sensors with an experience sampling application that measured Parkinson’s disease symptoms in daily life (Heijmans et al., 2019). The use of wearable sensors to detect PD symptoms is rapidly rising due to the lower costs, power efficiency, and accuracy of sensors. The sensors help detect tremors and bradykinesia, which are significant features of Parkinson’s disease. The surveillance was beneficial, and the results indicated that it is possible to identify Pd in the early stages and begin treatment early.
Measurable sensors were identified as a reliable method, and they relate well to the signs and symptoms of PD. The study used a simulated home setting, which gives a limited representation of the patients’ daily lives, making the study valid. Measuring the patient’s daily life increased the accuracy of results, which increased the reliability of the data presented. Regular clinical assessments are difficult to perform, leaving room for wearable sensors to do the job. The measuring system combined wearable sensors that measured acceleration with an experience sampling method (ESM) application. ESM is reliable because it has no recall bias, and data is collected multiple times daily.
The ESM consisted of questionnaires that contained questions about Parkinson’s disease symptoms. Patients wore the wearable sensors for 94% of the instructed timeframe, the response rate was high (71.9%), and the patients evaluated the monitoring system positively (Heijmans et al., 2019). The questionnaire showed that most participants found wrist (60%) and chest (80%) sensors comfortable to wear. The positions in which the patients wore the sensors were favorable because they were beneath clothes, and thus, fewer questions were asked in public about them. The findings were in the report, whose summary showed that introducing wearable sensors to patients with Parkinson’s disease was bound to bear good results.
Epidemiological Analysis of Parkinson’s Disease
Prevalence of Parkinson’s Disease
Epidemiology deals with the incidence distribution and possible control of diseases and other health factors. Epidemiology evolves with changes in society and the emergence of new ailments (Frerot et al.,2018). The 5Ws help examine the prevalence of Parkinson’s disease in a population. They refer to the who, what, where, when, and why, each representing person, item, place, time, and reason, respectively. The incidence of Parkinson’s disease increases with age, but an estimated 4% of people with the disease are diagnosed before age fifty (Marras et al., 2018). The last study done on PD in America was in 1978, and the results showed that the disease affected more men than women by over 1.5%. Men are known to engage in strenuous physical activities more than women do. Men are, therefore, more likely to experience nerve problems, especially when they overstrain their muscles or neglect the treatment of damaged muscles.
The study in North America was done to identify whether the prevalence of PD was uniform throughout the state or varied by study and geography. Parkinson’s disease affects people of advanced ages, such as fifty and above, which is evident because the number of people diagnosed with PD increases with age regardless of the sex of the patient (Marras et al., 2018). The data collected will be used to understand the disease and its prevalence further. The facts gathered about the ailment would be used by Parkinson’s Foundation to attract the attention of the state and pharmaceutical industry to the urgency of addressing PD.
Costs Associated with Parkinson’s Disease
Financial Costs
Approximately 60,000 Americans are diagnosed with PD yearly. However, PD incidence increases with age, and at least 4% of the people are diagnosed before age 50. With these numbers, the costs related to PD are projected to be high. Parkinson’s is the second most neurodegenerative disease after Alzheimer’s in the US, affecting nearly one million people (Marras et al., 2018). Approximately $ 2 billion per year is spent on the financial and social costs of Parkinson’s disease. Direct and indirect costs are incurred during the diagnosis of PD. Some direct financial costs included direct insurer and out-of-pocket costs (Martinez-Martin et al., 2018). Medication costs an average of $2,500 a year, while therapeutic surgery could cost $100,000 per person.
Social Costs
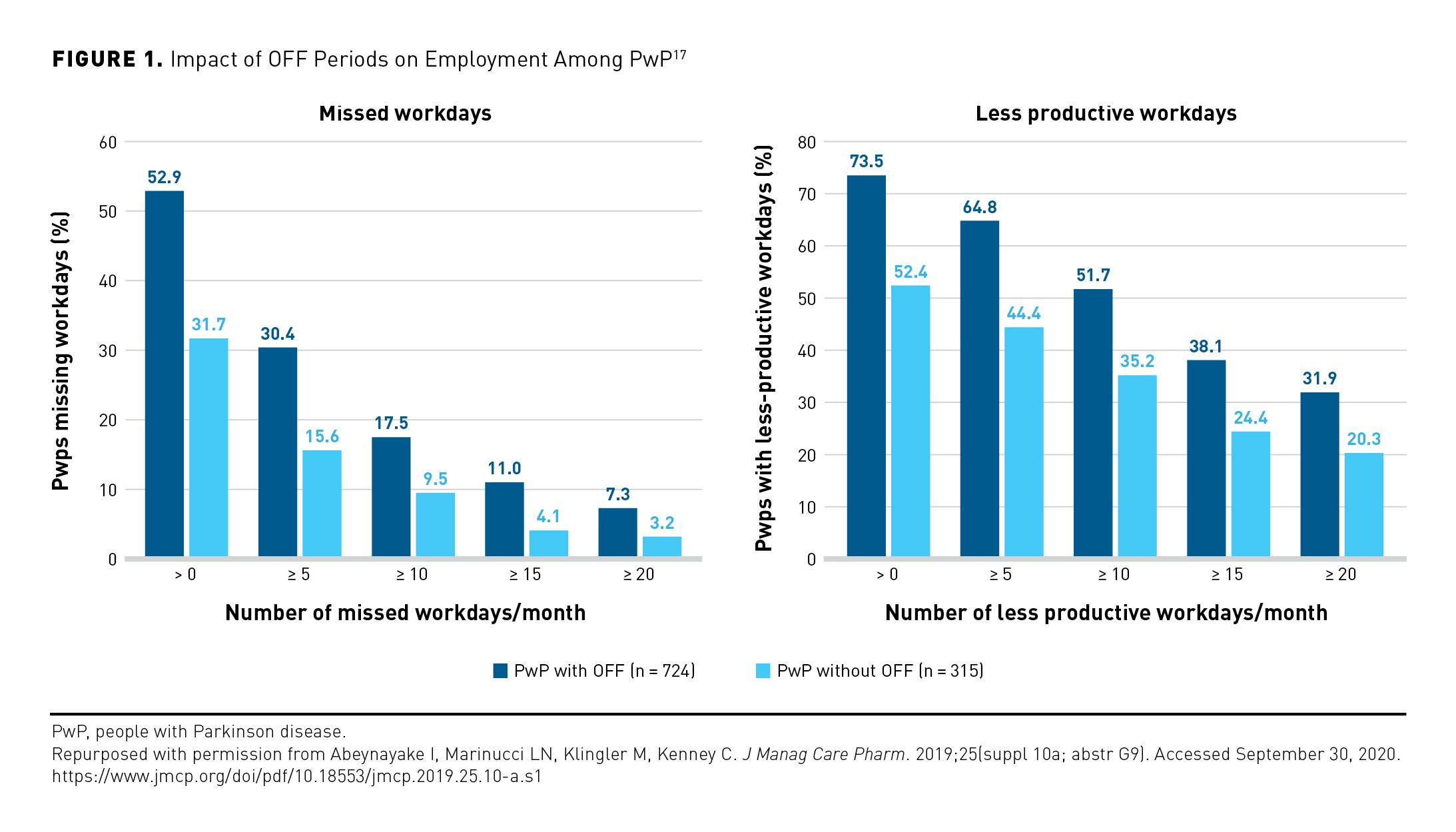
Note. PwP = People with Parkinson’s disease
As shown in Figure 1, PD affects the rate of absenteeism and the productivity of people going to work. The percentage of people with PD who took off days is higher than those without PD, and the percentage of people with low productivity due to PD is higher than those without PD. The table above shows that PD patients often missed work while others went to work, but their productivity was low. Among the indirect financial costs were future earning losses due to premature deaths, reduced employment, absenteeism and presenteeism, social productivity losses, and non-medical costs (Yang et al., 2020). Premature deaths occur when people with the disease cause accidents when they experience rigidity while driving. $7.5 billion was spent on non-medical costs such as home and motor vehicle modifications to accommodate patients with PD. $4.8 billion was spent due to disability income received by persons with PD (Yang et al., 2020). A combination of the financial and social costs of PD shows that the disease needs close monitoring as it demands a lot of money.
Screening, Diagnosis, and Guidelines on Parkinson’s Disease
Screening
Automation enabled fast accessibility, enhanced speed, and low usage costs of screening tools. The enhanced screening tools provided baseline information for neurologists while enabling them to identify potential PD patients before they visited the physicians. Screening refers to evaluating something to assess suitability for a particular role. The screening was made more accessible by the emergence of technology, which allowed the potential development of high-throughput screening tools (Chandra et al., 2021). The number of neurologists worldwide has been declining, which makes it necessary for patients to identify their symptoms before they need neurologists.
Additionally, PD screening was carried out through questionnaires where general questions about the signs and symptoms of the disease were asked. The questions focus on most daily activities involving movements such as reduction of speed in daily activities, reduction of the size of patient’s handwriting, difficulties in buttoning clothes, muscle stiffness, and feeling stuck on the chair while trying to get up. The questions were very relevant because PD is characterized by rigidity and bradykinesia. The answers given would help discover whether the patient has PD and begin the diagnosis immediately. Patients are expected to answer whether they have trouble with balancing and whether their peers and family members have noticed changes in their posture.
Diagnosis
Diagnosis involves identifying the nature of an illness by examining the symptoms. The most common method of diagnosing PD is through the symptoms identified by the patients or their caregivers. Doctors examine tremors, bradykinesia, rigidity, and posture instability. These are the fundamental symptoms associated with PD, and doctors combine them with other factors, such as family history and the environment, to increase the accuracy of identifying the disease as PD. Moreover, the DaTscan, an imaging scan, was identified as a technique that allowed doctors to see detailed pictures of the brain’s dopamine system (Hopkins, 2022). The scan involves the injection of a radioactive drug that binds with dopamine transmitters in the brain to show the location of dopaminergic neurons in the brain. The results of the scan help doctors confirm a diagnosis of PD.
Guidelines
Poor response to medical management poses a risk to PD patients, so health guidelines on managing the disease are necessary. Ultimately, PD becomes dominated by symptoms that respond poorly to medical management, and palliative care is needed (Heijmans et al., 2019). The National Institute of Health and Care Excellence (NICE) requires the provision of information about impulse control disorders, empowerment, and provision of information in ways that are accessible to patients and carers and prompt referral of the untreated patient to a specialist. These guidelines by NICE help physicians provide quality diagnosis and treatment to PD patients while ensuring that the patient’s quality of life is considered and upheld.
Medical Interventions for Parkinson’s Disease
The students understood the relevance of studies done and identified gaps and other sections that, when upheld well, would lead to better management of PD. People with PD who start exercising earlier experience a decline in quality of life compared to those who start later (Spears, 2022). The students could apply exercise as an intervention and develop a prescription system to help patients remember their medicine schedules and the type of medicine to take at specific times. Speech therapies play a crucial role in helping patients reduce stuttering and increase their confidence as they speak. The outcomes of these interventions are measurable because the students can see movement improvements and rigidity reduction in PD patients. Medications administered would help manage the systems, while speech therapy would assist the patient in communicating.
Conclusion
Various dimensions of Parkinson’s disease (PD) are examined, and the results enrich readers’ knowledge of managing the disease. The causes and symptoms, such as rigidity and bradykinesia, were expounded, the epidemiology and screening of PD were discussed, the diagnosis was recommended, and health guidelines were highlighted. Several medical interventions that could be done were elaborated, which would help nurses take care of PD patients while upholding a good quality of life for the patients. PD is a disease on which minimum research has been done, and it would be wise for more studies to be conducted to identify the specific cause of the disease.
References
Abeynayake, I., & Tanner, C. M. (2020). The economic impact of off periods in Parkinson’s disease. AJMC. [Table]. Web.
Chandra, J., Muthupalaniappan, S., Shang, Z., Deng, R., Lin, R., Tolkova, I., Butts, D., Sul, D., Marzouk, S., Bose, S., Chen, A., Bhaskar, A., Mantena, S., & Z.Press, D. (2021). Screening of Parkinson’s disease using geometric features extracted from spiral drawings. Brain sciences. Web.
Frérot, M., Lefebvre, A., Aho, S., Callier, P., Astruc, K., & Glélé, L. S. A. (2018). What is epidemiology? Changing definitions of epidemiology 1978-2017. PLOS ONE. Web.
Heijmans, M., Habets, J. G. V., Herff, C., Aarts, J., Stevens, A., Kuijf, M. L., & Kubben, P. L. (2019). Monitoring Parkinson’s disease symptoms during daily life: A feasibility study. Nature News. Web.
Hopkins. (2022). Parkinson’s disease risk factors and causes. Parkinson’s Disease Risk Factors and Causes | Johns Hopkins Medicine. Web.
Marras, C., Beck, J. C., Bower, J. H., Roberts, E., Ritz, B., Ross, G. W., Abbott, R. D., Savica, R., Van Den Eeden, S. K., Willis, A. W., & Tanner, C. M. (2018). Prevalence of Parkinson’s disease across North America. Nature News. Web.
Martinez-Martin, P., Macaulay, D., J.Jalundhwala, Y., Mu, F., Ohashi, E., Marshall, T., & Sail, K. (2018). The long-term direct and indirect economic burden of Parkinson’s. National Library of Medicine. Web.
NINDS. (2022). Tremor fact sheet. National Institute of Neurological Disorders and Stroke. Web.
Spears, C. (2022). Exercise. Parkinson’s Foundation. Web.
The admin. (2022). 2018 NICE guidelines for Parkinson’s disease. Hospital Healthcare Europe. Web.
WHO. (2022). Parkinson disease. World Health Organization. Web.
Yang, W., L.Hamilton, J., Kapil, C., C.Beck, J., M.Tanner, C., L.Albin, R., Dorse, E. R., Dahodwala, N., Cantina, I., Hogan, P., & Thompson, T. (2020). Current and projected future economic burden of Parkinson’s disease in the US NPJ Parkinson’s disease. Web.

