Introduction
Metabolic syndrome (MetS) is a group of risk factors, the combination of which can significantly threaten human health. According to the American Heart Association, 47 million Americans have this condition, more than 16 percent of the US population (Robinson, 2021). Metabolic syndrome occurs even more frequently in people with type 1 diabetes mellitus, among whom, according to a study by Belete et al. (2021), MetS prevalence reaches 25.9 percent. Among the components of metabolic syndrome are such common factors as high blood pressure or imbalance in cholesterol levels (Robinson, 2021). The latter aspect, in turn, may indicate the presence of dyslipidemia – the lack of an average balance between lipids in human blood.
This condition can lead to various diseases, from atherosclerosis to heart attacks. However, its detection is complicated by the small number of symptoms and their mild severity, and therefore they can be ignored by patients (Huizen, 2018). Recently, there has been a growing body of research on the relationship between vitamin D levels and human blood lipid levels: high and low-density lipids (HDL and LDL), total cholesterol (TC), and triglycerides (TGs). Confirmation of such an association would allow regulation of dyslipidemia, including in patients with MetS, by influencing vitamin D, often taken in the form of various supplements. Consequently, this research paper aims to investigate the impact of human vitamin D status on the lipid profile in patients with metabolic syndrome. Within this goal’s framework, the relationship of the vitamin with HDL, LDL, TC, TGs, and the mechanisms through which this interaction is carried out will be investigated.
Methodology
The central methodology of this study is a literature review of current research on the relationship between vitamin D and lipid profile in patients with MetS. These works were searched using scientific databases such as PubMed, APA PsycInfo, and Google Scholar. The keywords for querying were “vitamin D deficiency,” “lipid profile,” and “metabolic syndrome.” Another additional search criterion was the time of the research work: the period between them should not be more than ten years. Thus, the earliest articles in this literature review date back to 2012, which provides a sufficient level of relevance in current conditions.
In addition, this study only focused on original studies, and various types of reviews, including systematic and meta-analyses, were excluded from the final selection. Using such criteria made it possible to select 14 works, of which nine are observational, and five are experimental. The identified studies were thus divided into two categories, presented in tables in the Results section. Each of these works was examined in detail according to the critical parameters indicated in the table, based on which the final results were compiled.
Results
Table 1. Observational Studies
Table 2. Experimental Studies
Vitamin D and Total Cholesterol
Among the reviewed observational articles in Table 1, most reported an inverse correlation between vitamin D and total cholesterol levels. However, the significance of these results is very low since only three studies have demonstrated a substantial enough correlation between these parameters based on the p-level. At the same time, the work of Skaaby et al. (2012) noted a slight increase in this parameter. Nevertheless, the changes in total cholesterol value are minimal, and the p-value, in this case, is 0.12 with a standard threshold of 0.05 (Skaaby et al., 2012). Therefore, the true nature of the interaction between vitamin D and TC is unclear based on evidence from observational studies. The number of significant results is insufficient to form an unambiguously positive opinion, but their presence does not allow a negative verdict to be made.
The experimental studies presented in Table 2 also show an ambiguous result regarding the relationship between vitamin D and TC. At first glance, there is more evidence in favor of lowering total cholesterol levels. However, the increase in total cholesterol in the study by Wenclewska et al. (2019) is statistically significant because its p-value is < 0.01. Thus, the evidence from experimental studies in some way contradicts observational studies, which further complicates the formation of an unambiguous opinion on this issue.
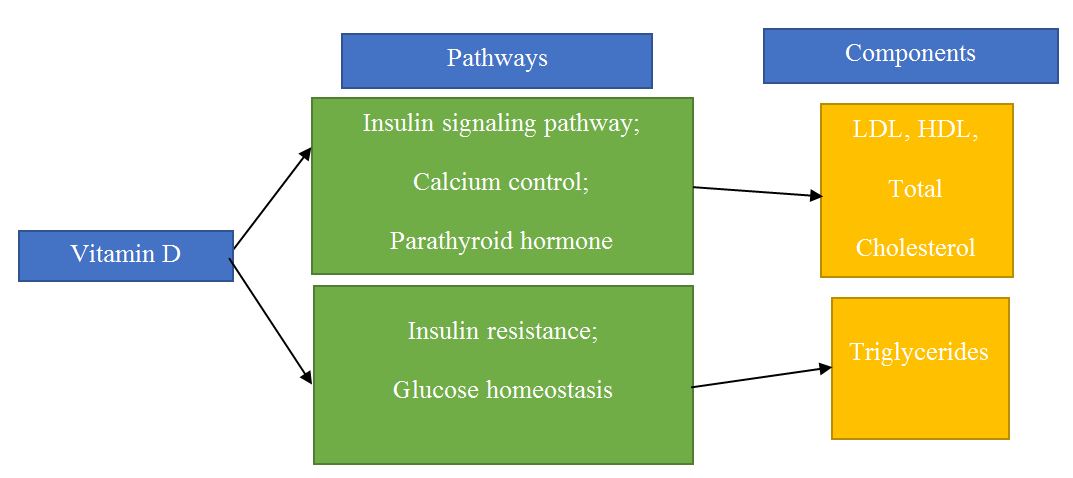
The effect on total cholesterol is influenced by the impact of its components, including HDL, LDL, and triglycerides. Therefore, among potential pathways, insulin signaling pathway, sex hormone control, and blood pressure control measures can be identified. However, the most likely management options concerning the lipid profile remain the calcium and parathyroid hormone (PTH) levels (Skaaby et al., 2012). An inverse association exists between vitamin D, explicitly circulating 25(OH)D levels, and PTH, where increased vitamin D levels enhance intestinal calcium absorption efficiency by about 30-40%, reducing PTH secretion by the parathyroid gland (Pascale et al., 2018). Nonetheless these observations are yet to be confirmed, as population studies did not show independent associations between PTH and serum lipid levels or hyperlipidemia risk (Chen et al., 2014; Landin-Wilhelmsen et al., 1995). Therefore, to fully explain these relationships, it is necessary to investigate additional pathways that affect lipid levels, both individually and in general.
Vitamin D and LDL
Virtually all the observational studies reviewed have noted some association between vitamin D and LDL. Except for the work by Skaaby et al. (2012), the detected effects belonged to the category of inverse correlation. However, Skaaby et al. (2012) did not show significant results in this context, as the p-value is 0.38. On the other hand, almost half of the studies examined confirmed the feedback with results of substantial statistical importance. Such a distribution among the results of the studies suggests that in this context, there is considerable evidence in favor of the inverse correlation of the studied parameters.
Nevertheless, experimental studies do not support this observation, as their results show much more diversity. For example, Makariou et al. (2017) and Wenclewska et al. (2019) indicate an increase in these lipoprotein levels. However, the results of all these experiments cannot be considered statistically significant due to the too high p-value. Therefore, although the body of evidence suggests an inverse relationship between vitamin D supplementation and LDL, it needs further verification and analysis.
The LDL-lowering effects of vitamin D may be of clinical significance in reducing the risk of cardiac events. In isolated monocytes from patients with type 2 diabetes mellitus, vitamin D supplementation resulted in a reduced LDL-C uptake by circulating monocytes (Riek et al., 2018). According to Surdu et al. (2021), it reduces atherosclerosis risk through decreased transport into the walls of blood vessels. Various pathways may explain the relationship between vitamin D and LDL, such as the insulin signaling pathway and maintaining glucose homeostasis (Wenclewska et al., 2019). Furthermore, the effect on calcium control and parathyroid hormone suppression is also a theoretical pathway (Skaaby et al., 2012). Still, the particular mechanisms of vitamin D interaction with lipids remain not fully understood.
Vitamin D and HDL
Observational studies have indicated greater agreement between results in the context of HDL and vitamin D. While some investigations have failed to establish any relationship, the rest claim a direct correlation. However, their validity is questionable as none of these sources show statistically significant results. Thus, the current trend towards a positive relationship requires additional confirmation and study. Experimental work, however, shows approximately the same results. Except for the study by Kelishadi et al. (2014), all papers state a direct correlation between vitamin D and HDL. However, only the result of Wenclewska et al. (2019), for which the p-value is less than 0.001, can be considered significant. Therefore, based on the investigations data, it is impossible to make an unambiguous answer about the relationship of variables, but the presence of a positive trend is evident.
The inverse association between vitamin D and HDL levels was previously confirmed in other population studies, which also has implications for modifying the atherosclerosis process (Karhapää et al., 2010). However, as in the case of LDL, the exact nature of the relationship between vitamin D and HDL remains incomplete. The reviewed literature highlights the effects of vitamin D on multiple functions and its close association with various metabolic pathways (Wieder-Huszla et al., 2019). The insulin signaling pathway also seems to be an essential control mechanism (Scmitt et al., 2018). Nevertheless, the path most closely identified is the regulation of calcium levels and the suppression of parathyroid hormone, as in the case of LDL (Skaaby et al., 2012). In addition, the literature makes it possible to identify the simultaneous influence of these pathways and their joint significance.
Vitamin D and Triglycerides
Observational studies on the relationship between vitamin D and triglycerides show some of the most consistent and consistent results. As can be seen from Table 1, the vast majority of studies identify the presence of a negative correlation between these variables. In addition, almost half of the papers show statistically significant results with p-values less than 0.05. With the vast majority of investigations showing similar effects, it is safe to conclude that there is evidence for an inverse relationship between vitamin D and TGs.
In the context of experimental studies, the stability of the observed results is somewhat lower. Following the investigation of Wenclewska et al. (2019), there is a positive correlation between vitamin D and triglycerides, which, however, is not significant. On the other hand, more than half of the papers presented in Table 2 demonstrate confirmed statistical inverse correlation. Therefore, it is possible to conclude that the interaction of triglycerides with vitamin D is somewhat more straightforward and, with a high degree of probability, indeed has an inverse correlation.
The association is best explained by the effect of vitamin D on insulin resistance. According to Kelishadi et al. (2014), this mechanism provokes inflammatory cytokine production, which is directly associated with obesity and, as a result, triglycerides, which are major components of human body fat. In addition, the relationship between vitamin D and glucose tolerance may be a potential explanation (Baker et al., 2012). Another mechanism may be connected with calcium absorption, including the effect of lower potential calcium content in the gut, related to enhanced vitamin D status, which reduces calcium binding to free fatty acids and the formation of insoluble soaps. This effect increases the absorption of fatty acids and, consequently, blood triglycerides levels (Schwetz et al., 2018). Oral calcium has been shown previously to promote reductions in triglycerides levels (Papageorgiou et al., 2022; Sein et al., 2014).
Discussion
The papers studied in this literature review allow noting several vital details. First of all, only a small part of the analyzed articles shows significant results. Moreover, their relevance often decreases with the application of additional analysis and correlation test methods, as in the case of Wenclewska et al.’s study (2019). The presence of this factor greatly complicates obtaining any detailed picture of the relationship between vitamin D and the lipid profile.
However, within this paper, several common associations were identified that are worth analyzing in more detail. Although the results of many studies are insignificant, there is a steady trend for each parameter. This is especially noticeable in the observational studies presented in Table 1 due to their number. Most papers incline on the same result, while the number of studies that gave opposite results is minimal. This trend is less visible in experimental studies due to their small number. However, the general trends in both observational and experimental papers coincide. Such results do not allow stating an unambiguous relationship between particular components but make it possible to assume a propensity for one or another behavior.
Thus, a general analysis of the results of the studied papers shows that vitamin D is directly related to HDL levels but inversely related to other components of the lipid profile – LDL, TC, and TGs. Such a connection, at first glance, can be explained using the well-established understanding of HDL as a “useful” element (Xiang & Kingwell, 2019). However, such reasoning can be opposed both by the modern scientific base, which testifies to more complex mechanisms of the HDL, and by the significant results of the work of Schmitt et al. (2019) emphasizing inverse correlation. In the context of HDL, there is some ambiguity in the considered works since significant observational and experimental evidence indicates opposite dependencies.
Research on LDL, however, shows a more robust inverse relationship with vitamin D, which is consistent with the perception of this component as “bad” cholesterol. However, such different results for HDL and LDL only complicate the analysis of total cholesterol since both parts must influence it. The most evident trend in this context is the inverse relationship between TGs and vitamin D, as many significant results have been found to signal this.
Such trends can theoretically be explained by analyzing various metabolic pathways. Nevertheless, the studied papers make it almost impossible to clearly define the mechanisms of interaction between vitamin D and lipid profile components. One study directly states that, according to the current literature, the interaction of these elements is not clear enough (Skaaby et al., 2012). However, most research agrees that insulin resistance and the effects on lipids through calcium levels play a prominent role in this connection. The relationship between vitamin D and TGs can also be explained by the positive impact of the former on inflammatory cytokine production. Since there is a significant increase in inflammatory processes in obesity, their reduction can positively affect this condition and, as a result, the level of fats – triglycerides. However, within this paper’s framework, it is impossible to accurately state the mechanisms of interaction between the studied components and unambiguously establish the relationship between them.
Limitations
Such results and the inability to draw a definitive conclusion can be explained by the limitations that faced this study. First, it is worth noting a small number of sources used for literary analysis. This is most clearly seen in the number of experimental papers studied, the number of which does not even allow one to determine the trend without significant results adequately. In this context, as a limitation, one can also single out the search criteria, which, in theory, could limit the ability to identify articles relevant to the work. Criteria, in this case, means both keywords and the restriction of the scope of the search only to original studies. Finally, another limitation is the lack, in many cases, of explanations regarding the working mechanisms in the reviewed research papers. Although they are focused on identifying the relationship, the authors of the articles mostly did not try to explain in detail the essence of these phenomena.
Recommendations
Several recommendations for further research can be made based on the identified limitations. First, a more extensive and detailed literature analysis is needed to obtain more reliable results. It should include more material, allowing researchers to track trends and objectively identify more significant effects. Optimal literature search methods should be used to accomplish this task, including more precise queries and access to specialized databases. Secondly, in subsequent investigations, it is recommended to separate the tasks facing the study, focusing either on the study of metabolic pathways or determining the effect of vitamin D on the components of the lipid profile. As practice shows, these two tasks do not intersect well in the literature and require an individual approach to each of them to obtain reliable results. Finally, another recommendation for research can be the further development of this topic and the analysis of the effect of vitamin D on other components of metabolic syndrome.
Conclusion
Thus, the conducted study allows stating that in modern literature, there are conflicting opinions about the relationship between vitamin D and the components of the human lipid profile. Significant results were found for some of the studied parameters, declaring the presence of associations of the opposite kind. In this regard, a full-fledged analysis of the principles of the influence of vitamin D is complicated, and an unambiguous definition of the mechanism of action in this paper seems impossible. However, based on the data collected, it can be concluded that vitamin D tends to be directly related to HDL in human blood and inversely related to LDL, TC, and TGs. Nevertheless, this information needs further verification and confirmation through more extensive, accurate, and qualitative studies. In addition, there is a need to determine the mechanism of action of vitamin D on these elements since, at the moment, this issue has not been fully clarified. Therefore, this study can be considered as the first step toward a full-fledged analysis of this problem.
References
Ahmadi, F., Damghani, S., Lessan‐Pezeshki, M., Razeghi, E., Maziar, S., & Mahdavi‐Mazdeh, M. (2016). Association of low vitamin D levels with metabolic syndrome in hemodialysis patients. Hemodialysis International, 20(2), 261-269. Web.
Alkhatatbeh, M. J., Abdul-Razzak, K. K., Khasawneh, L. Q., & Saadeh, N. A. (2017). High prevalence of vitamin D deficiency and correlation of serum vitamin D with cardiovascular risk in patients with metabolic syndrome. Metabolic Syndrome and Related Disorders, 15(5), 213-219. Web.
Baker, J. F., Mehta, N. N., Baker, D. G., Toedter, G., Shults, J., Von Feldt, J. M., & Leonard, M. B. (2012). Vitamin D, metabolic dyslipidemia, and metabolic syndrome in rheumatoid arthritis. The American Journal of Medicine, 125(10), 1036-e9. Web.
Barbalho, S.M., Tofano, R.J., de Campos, A.L., Rodrigues, A.S., Quesada, K., Bechara, M.D., de Alvares Goulart, R., Oshiiwa, M. (2018). Association between vitamin D status and metabolic syndrome risk factors. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 12(4), 501-507. Web.
Chen, W. R., Sha, Y., Chen, Y. D., Shi, Y., Yin, D. W., & Wang, H. (2014). Vitamin D, parathyroid hormone, and serum lipid profiles in a middle-aged and elderly Chinese population. Endocrine Practice, 20(6), 556–565. Web.
Ferreira, P. P., Cangussu, L., Bueloni-Dias, F. N., Orsatti, C. L., Schmitt, E. B., Nahas-Neto, J., & Nahas, E. A. P. (2020). Vitamin D supplementation improves the metabolic syndrome risk profile in postmenopausal women. Climacteric, 23(1), 24-31. Web.
Fu, J., Han, L., Zhao, Y., Li, G., Zhu, Y., Li, Y., Li, M., Gao, S., & Willi, S.M. (2019). Vitamin D levels are associated with metabolic syndrome in adolescents and young adults: The BCAMS study. Clinical Nutrition, 38(5), 2161-2167. Web.
Karhapää, P., Pihlajamäki, J., Pörsti, I., Kastarinen, M., Mustonen, J., Niemelä, O., & Kuusisto, J. (2010). Diverse associations of 25-hydroxyvitamin D and 1,25-dihydroxy-vitamin D with dyslipidaemias. Journal of Internal Medicine, 268(6), 604–610. Web.
Kelishadi, R., Salek, S., Salek, M., Hashemipour, M., & Movahedian, M. (2014). Effects of vitamin D supplementation on insulin resistance and cardiometabolic risk factors in children with metabolic syndrome: A triple-masked controlled trial. Jornal de Pediatria, 90(1), 28-34. Web.
Landin-Wilhelmsen, K., Wilhelmsen, L., Lappas, G., Rosen, T., Lindstedt, G., Lundberg, P.A., Wilske, J., & Bengtsson, B.Å. (1995). Serum intact parathyroid hormone in a random population sample of men and women: Relationship to anthropometry, life-style factors, blood pressure, and vitamin D. Calcified Tissue International, 56(2), 104-108. Web.
Makariou, S. E., Elisaf, M., Challa, A., Tentolouris, N., & Liberopoulos, E. N. (2017). No effect of vitamin D supplementation on cardiovascular risk factors in subjects with metabolic syndrome: A pilot randomised study. Archives of Medical Sciences. Atherosclerotic Diseases, 2, e52. Web.
Papageorgiou, M., Merminod, F., Ferrari, S., Rizzoli, R., & Biver, E. (2022). Associations of calcium intake and calcium from various sources with blood lipids in a population of older women and men with high calcium intake. Nutrients, 14(6), 1314. Web.
Pascale, A. V., Finelli, R., Giannotti, R., Visco, V., Fabbricatore, D., Matula, I., Mazzeo, P., Ragosa, N., Massari, A., Izzo, R., Coscioni, E., Illario, M., Ciccarelli, M., Trimarco, B., & Iaccarino, G. (2018). Vitamin D, parathyroid hormone and cardiovascular risk: The good, the bad and the ugly. Journal of Cardiovascular Medicine (Hagerstown, Md.), 19(2), 62–66. Web.
Riek, A. E., Oh, J., Darwech, I., Worthy, V., Lin, X., Ostlund, R. E., Zhang, R. M., & Bernal-Mizrachi, C. (2018). Vitamin D3 supplementation decreases a unique circulating monocyte cholesterol pool in patients with type 2 diabetes. The Journal of Steroid Biochemistry and Molecular Biology, 177, 187–192. Web.
Salekzamani, S., Mehralizadeh, H., Ghezel, A., Salekzamani, Y., Jafarabadi, M. A., Bavil, A. S., & Gargari, B. P. (2016). Effect of high-dose vitamin D supplementation on cardiometabolic risk factors in subjects with metabolic syndrome: A randomized controlled double-blind clinical trial. Journal of Endocrinological Investigation, 39(11), 1303-1313. Web.
Schmitt, E. B., Nahas-Neto, J., Bueloni-Dias, F., Poloni, P. F., Orsatti, C. L., & Nahas, E. A. P. (2018). Vitamin D deficiency is associated with metabolic syndrome in postmenopausal women. Maturitas, 107, 97-102. Web.
Schwetz, V., Scharnagl, H., Trummer, C., Stojakovic, T., Pandis, M., Grübler, M. R., Verheyen, N., Gaksch, M., Zittermann, A., Aberer, F., Lerchbaum, E., Obermayer-Pietsch, B., Pieber, T. R., März, W., Tomaschitz, A., & Pilz, S. (2018). Vitamin D supplementation and lipoprotein metabolism: A randomized controlled trial. Journal of Clinical Lipidology, 12(3), 588-596.e4. Web.
Sein, M. T., Latt, T. S., & Ohnmar -. (2014). Effect of oral calcium supplementation on lipid profile and atherogenic index of plasma. Journal of the ASEAN Federation of Endocrine Societies, 29(2), 135–135.
Skaaby, T., Husemoen, L. L. N., Pisinger, C., Jørgensen, T., Thuesen, B. H., Fenger, M., & Linneberg, A. (2012). Vitamin D status and changes in cardiovascular risk factors: A prospective study of a general population. Cardiology, 123(1), 62-70. Web.
Surdu, A. M., Pînzariu, O., Ciobanu, D.-M., Negru, A.-G., Căinap, S.-S., Lazea, C., Iacob, D., Săraci, G., Tirinescu, D., Borda, I. M., & Cismaru, G. (2021). Vitamin D and its role in the lipid metabolism and the development of atherosclerosis. Biomedicines, 9(2), 172. Web.
Wang, Y., Si, S., Liu, J., Wang, Z., Jia, H., Feng, K., Sun, L., & Song, S. J. (2016). The associations of serum lipids with vitamin D status. PLoS One, 11(10), e0165157. Web.
Wenclewska, S., Szymczak-Pajor, I., Drzewoski, J., Bunk, M., & Śliwińska, A. (2019). Vitamin D supplementation reduces both oxidative DNA damage and insulin resistance in the elderly with metabolic disorders. International Journal of Molecular Sciences, 20(12), 2891. Web.
Wieder-Huszla, S., Jurczak, A., Szkup, M., Barczak, K., Dołęgowska, B., Schneider-Matyka, D., Owsianowska, J., & Grochans, E. (2019). Relationships between vitamin d3 and metabolic syndrome. International Journal of Environmental Research and Public Health, 16(2), 175. Web.
Xiang, A. S., & Kingwell, B. A. (2019). Rethinking good cholesterol: a clinicians’ guide to understanding HDL. The Lancet Diabetes & Endocrinology, 7(7), 575-582. Web.

