HCAHPS Scores
My hospital of choice for analyzing HCAHPs scores is Abbott Northwestern Hospital that is situated in Minneapolis, Minnesota. It is the largest not-for-profit facility serving the Twin Cities and the Upper Midwest communities. As indicated in the Hospital Compare website, Abbott Northwest Hospital’s (ABH) overall HCAHPS score is 4/5 (Medicare.gov, 2020a). The four star rating means ABH delivers above average quality for each measure examined.
State and National Averages
The HCAHPS data on a variety of items for ABH and the Minnesota and national averages are shown in Table 1.
Table 1: HCAPS Data for ABH Compared to State and National Averages.
The table indicates that ABH performed better than the Minnesota and national averages in two of the 10 HCAHPS scores: ‘hospital rating of 9 or 10’ and ‘would definitely recommend’ (Medicare.gov, 2020a). Its performance in ‘understood their care when they left the hospital’ was the same as the Minnesota mean score. ABH surpassed the national average on three items: ‘nurses “always” communicated well’, ‘doctors “always” communicated well’, and ‘understood their care when they left the hospital’.
Comparison to Other Hospitals
The two nearby hospitals (within a fifty-mile radius in Minneapolis) are North Memorial Health and Park Nicollet Methodist. Their HCAHPS data and those of ABH are indicated in Table 2.
Table 2: HCAHPS Data for ABH Compared to Two Other Hospitals.
From the table, ABH performs better than both North Memorial Health and Park Nicollet Methodist Hospital in four key HCAHPS measures. It outperforms the two facilities in nurse and physician communication, room and bathroom hygiene, and provision of discharge instructions. However, its performance is lower than that of the two nearby hospitals in one measure: ‘area around their room was “always” quiet at night (Medicare.gov, 2020a). Paired comparisons show that ABH outperforms North Memorial Health in eight measures. It scores lower than Park Nicollet Methodist Hospital in four areas and ties in two domains. This comparative analysis suggests that ABH is the best acute care hospital in Minneapolis in patient experience but Park Nicollet Methodist Hospital is a strong competitor.
Survey Response Rates
The rate and number of surveys for ABH, North Memorial Health, and Park Nicollet Methodist Hospital are shown in Table 3. These facilities have a four-star, three-star, and four-star ratings, respectively. The response period for the data indicated is one year.
Table 3: Survey Response Rates.
ABH’s response rate is higher than that of North Memorial Health but low compared to Park Nicollet Methodist Hospital’s completion level. Similarly, more patients in ABH completed the surveys upon discharge compared to the participants in North Memorial Health’s evaluation. However, this number is lower compared to that recorded by Park Nicollet Methodist Hospital, suggesting that it serves a larger patient mix or has bigger bed capacity than ABH.
Demographics and Services Provided
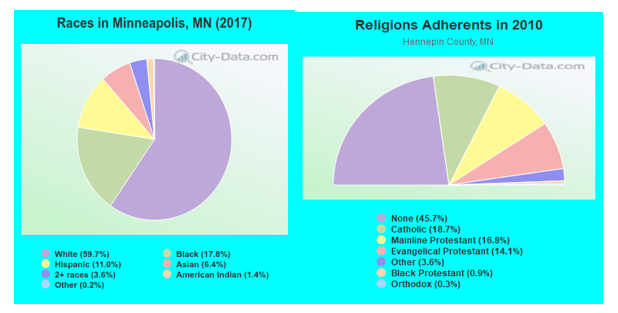
ABH is an acute care hospital that primarily serves communities living in Minneapolis, Minnesota (Zip Code 55401-55488). This city’s population of 422,331 is predominantly White (59.7%) followed by Black (17.8%) and Hispanic (11.0%) (City-data.com, 2021). The cultural values and beliefs are comparable to the national culture but with strong Scandinavian, Finnish, Irish, and German influences from migrants. They are deep family ties and shared emotional connection among residents. A large proportion of the population is not religious, with 18.7% and 16.8% of the people professing Catholic and Protestant religions, respectively (City-data.com, 2021). The most spoken language is English but minority groups also use Spanish.
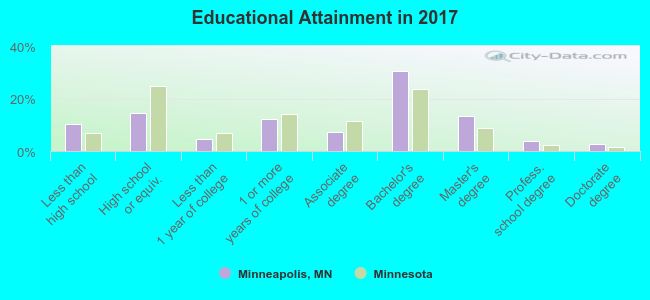
Minneapolis population is among the top educated demographic in Minnesota. For people aged 25 years and over, 89.6% of them have attained high school or higher, 50.8% have a Bachelor’s degree, 20.2% possess a graduate or professional training, and 5.8% are unemployed (City-data.com, 2021). These statistics suggest a higher college completion rates in this city. However, high school attainment in Minneapolis is lower than the state average (Figure 2).
The socioeconomic profile of Minneapolis reflects interesting insights into healthcare access and utilization. The unemployment rate stands at 5.8%, while the median household income is $60,789 per annum compared to the Minnesota average of $68,388 (City-data.com, 2021). Incomes have grown steadily since 2,000, which suggest a robust economy. However, unemployment is bound to increase dramatically due to the economic effects of the global pandemic.
ABH provides a broad range of services to Minneapolis communities, such as inpatient, outpatient, and acute care. A comprehensive list of the specific options available at the facility, including specialty care, is given below (City-data.com, 2021):
- Mental health and addiction services
- Heart and vascular care
- Neurological care
- Orthopedic prevention, diagnosis, and treatment
- Integrative/alternative medicine
- Comprehensive rehabilitative services
- Treatment of spinal diseases and disorders
- Surgical services
- Reproductive healthcare
- Cancer diagnosis, prevention, and treatment.
ABH delivers these services through a network of clinics and institutes to meet population needs. Specialty inpatient and outpatient care is offered through a range of medical centers, including the Minneapolis Heart Institute, Orthopedic Institute, and WomenCare. The patients served include those with unique needs such as mental and addiction disorders, heart conditions, neurological disorders, and spine diseases. ABH also treats the reproductive health needs of women across all ages.
Cultural Dynamics
Patient-reported healthcare experience depends on the characteristics of the community served. For ABH, racial/ethnic composition is a patient-specific factor impacting its HCAHPS scores. The higher percentages of whites in the zip codes served by ABH could lead to favorable HCAHPS ratings, as they may not experience communication or language barriers like Hispanic (Spanish speakers) and African American (African languages) patients do. On the other hand, a healthcare staff comprising fewer minority groups could potentially impact hospital experiences of Latino/black patients. As a result, they are likely to rate the hospital poorly on communication-related HCAHPS components, for example, nurse and physician communication, staff responsiveness, instructions about medicines, and discharge information.
B6B. Educational Dynamics
Patients with low or high educational attainment may experience healthcare differently or have dissimilar expectations. The population in the zip codes served by ABH has a relatively high education level (college completion rates), so it expects more from the hospital staff, potentially affecting HCAHPS scores. Educated patients need to be kept informed and may be less tolerant to delays in care delivery. This scenario could negatively affect staff responsiveness and communication-related HCAHPS components, such as physician and nurse communication and discharge instructions. Tech-savvy consumers may expect the staff to use interactive and self-service tools to engage them better, which could potentially decrease the overall hospital rating and recommendation, if their expectations are not met.
Socioeconomic Dynamics
Socioeconomic factors potentially affecting ABH’s HCAHPS scores include income and unemployment rate. The areas served have lower median income than the Minnesota average. Thus, this population is less affluent, implying that their expectations of response time, staff communication, and hospital environment may be low. The middle-income patients could potentially increase the responsiveness, quietness, and cleanliness HCAHPS questions as they do not expect higher standards than the staff can deliver. In addition, their overall rating of the hospital and recommendation may increase, as the hospital care would match their expectations.
Financial Impact
Table 4: Short-term and Long-term Financial Impact of Poor HCAHPS Scores.
Lower HCAHPS scores than those of nearby hospitals could affect ABH financially under the value-based purchasing program. A potential short-term impact on the hospital’s bottom line is a reduced number of patients served because they are not satisfied with the services offered. A poor HCAHPS rating would hurt a facility’s quality reputation, forcing consumers to opt for a different provider. In the short term, low consumer loyalty could impact utilization of a facility’s services because of reduced hospital recommendations to families. Furthermore, poor inpatient experience could potentially increase staff turnover because of the pressure to improve rating.
The long-term financial impacts are related to reductions in regular Medicare payments, if the HCAHPS scores are lower than the state and national averages. As patient experience accounts for a large percentage of value-based incentives, low ratings are likely to attract financial penalties from payers.
Impact on Quality
Table 5: Impact of Poor HCAHPS Scores on Quality.
Low HCAHPS scores can impact quality and safety outcomes at the hospital. For example, ineffective nurse or physician communication is likely to affect care planning and decision-making about treatments. It would reduce the use of safety and confidentiality information. Additionally, poor HCAHPS ratings in components such as communication about medicines and discharge information would decrease patient adherence to clinical guidelines, increasing readmissions, length of stay, and inpatient mortality. The pressure to improve low HCAHPS scores may have unintended consequences on quality. It may lead to cosmetic responses to boost ratings, for example, providing entertainment to patients. As a result, the quality of care is likely to decline. Focusing on improving the inpatient experience may also lead to inappropriate care, including yielding to unreasonable requests on drug prescriptions, which would compromise patient safety.
Causes of Scores
Table 6: Causes of Poor HCAHPS Scores.
ABH ranks below the national average four of the HCAHPS items. The three poorly rated HCAHPS questions are nurse and physician communication, staff responsiveness, and discharge information. A number of reasons could account for the low scores in the first item. First, a disengaged nursing staff is likely to affect communication with patients and responsiveness. Second, poor communication skills among nurses and physicians due to a lack of training may contribute to their limited efficacy to engage patients. Third, ABH’s technology investments probably do not support effective interaction with inpatients – from setting appointments to follow-ups.
The three probable causes of low staff responsiveness scores include unmet patient expectations (being mindful of time), failure by caregivers to anticipate inpatient needs, and difficulty reaching staff via phone or other media, resulting in delayed care. The patients require nurses to be responsive to their needs and assuring to reduce anxiety. The potential causes of low scores on the discharge information question are the difficulty reading or understanding instructions due to the complex terminologies used, low health literacy among patients, and limited pre-discharge preparation. As a result, patients are unaware of post-hospitalization care needs at discharge.
Organizational Change
Table 7: Organizational Change to Improve Scores.
The organizational changes proposed will address each of the three selected HCAHPS questions. A communication policy that includes training will enable staff to engage with patients, increase shared decision-making, and dispel any fears or concerns. Investing in new interactive technology (reminders and alerts) will enhance staff responsiveness to inpatient needs. Also, a teach-back technique and non-medical terms can enhance patients’ acknowledgment and understanding of the discharge information received.
Structure, Processes, and Outcomes
Table 8: Structure, Processes, and Outcomes of the Strategic Plan.
The low scores in nurse communication, responsiveness, and discharge information need to be improved. The methods (process) for achieving the desired outcome (better ratings in the three questions) include using shared governance (interdisciplinary SG council) to empower nurses in communication, literature search to develop EBP guidelines, and collaborating with physicians and nurses to implement the new policy and teach-back protocols. Additionally, working with IT, nurse training, and implementation of new technologies would improve HCAHPS scores in the three components.
Improving Organizational Quality
EBPs will be incorporated into the facility through nurse-led interventions and quality improvement projects at the point of care. Through organizational support, the nursing staff will learn and develop a culture of using the PICO approach to address practice gaps. Implementing shared governance at ABH will entail interdisciplinary SG councils that report regularly to all staff and share information on quality measures. Nurses will become more aware of quality measures tied to their role that affect hospital HCAHPS scores, enhancing their accountability and obligation to follow best practice guidelines.
D4. Shared Accountability
Technology Trends
Adopting new technologies, including electronic health records, at the facility will enhance communication with patients and among clinicians. Such systems will also reduce the risk of medication errors and enhance access to patient data to support patient-centered care. Technology and systems that send reminders and alerts to nurses will enhance staff responsiveness. Wearable devices and fitness trackers will be used to monitor blood pressure and sugar levels for prompt intervention.
Improve Care Delivery System
Table 12: Improving the Care Delivery System.
Improve Financial Stability
Improving the three HCAHPS scores will lead to a better overall hospital rating. As a result, the regular CMS payments to ABH will increase significantly, contributing to its financial stability. In addition, a quality reputation due to higher HCAHPS scores will contribute to market share growth. More admissions will result in revenue increases and quality service, due to low turnover of skilled staff to other hospitals in the region.
Stakeholder Roles and Responsibilities
Table 13: Shareholder Roles and Responsibilities.
Stakeholder Accountability and Involvement
Table 14: Stakeholder Accountability and Involvement.
Training
Table 15: Staff Training.
Plan Implementation
Table 16: A Timeline for Plan Implementation
Evaluate the Strategic Plan’s Success
Table 17: Process of Evaluating the Strategic Plan’s Success.
Involvement of Stakeholders
Table 18: Involvement of Key Stakeholders.
Communication of Results
Table 19: Communicating the Evaluations Results.
References
Allina Health. (n.d.). Services. Web.
City-data. (2021). Minneapolis, Minnesota. Web.
Medicare. (2020a). Hospitals. Web.
Medicare. (2020b). Abbott Northwestern Hospital: Patient survey rating. Web.
Medicare. (2020c). North Memorial Health: Patient survey rating. Web.
Medicare. (2020d). Park Nicollet Methodist Hospital: Patient survey rating. Web.

