Abstract
Hospital acquired Pressure Injuries (HAPIs) are not a new issue in the healthcare industry, meaning that they can be viewed historically. HAPIs are costly to the healthcare system and mostly preventable, yet incidence rates remain high. Recommendations for improved care and prevention of pressure injuries from the Joint Commission revolve around continuous monitoring of prevention protocols and prompts for the care team. The purpose of this quantitative, quasi-experimental project was to determine if or to what degree the implementation of Pressure Injury Prevention (PIP) Bundle impacts the HAPIs prevalence rate among critical care patients in acute care hospital over four-weeks. Jean Watson’s Human caring nursing theory is used in this DPI project to identify how PIP bundle can be associated with reduced HAPI incidence. The sample population for this project will be minimum 60 adult patients. The HAPI incidence is the project’s dependent variable, and it is necessary to compare this value for two independent groups. The collected data will be analyzed by utilizing the t-test, since this inferential statistical test measures the difference between the means of two groups. The specific level of the statistical significance (p<.05) is chosen to ensure that the obtained results are statistically significant and minimize the effect of chance. This requirement is also necessary because it justifies that the findings are scientifically valuable. It is anticipated that utilization of PIP bundle can reduce the pressure injuries among adult critical care patients.
Introduction to the Project
Hospital-acquired pressure injuries (HAPI) are a significant burden for healthcare organizations worldwide that negatively impacts the quality of life of patients and their caregivers. The global prevalence of HAPI is almost 13%, while the incidence rate is above 5 per 10,000 patient days (Li et al., 2020). Most cases of HAPI are preventable; however, highly cachectic patients may develop pressure injuries despite the use of cushions for pressure distribution (Ricci et al., 2017). In addition to being a stressful event for patients, HAPI is also a formidable financial burden because most pressure ulcers develop as a secondary condition, requiring additional expenses (Mansfield et al., 2019).
For example, according to national estimates, the overall spending for treating patients with HAPIs is close to $11 billion (Padula & Delarmente, 2019). The HAPI prevalence in the 13-bed medical intensive care unit (MICU) in urban New York was reported to be 14%, which is higher than the national average. Therefore, this direct practice improvement (DPI) project aims to determine how implementing evidence-based practices, the pressure injury prevention bundle, can reduce the HAPI incidence in the 13-bed MICU.
Although many evidence-based methods were developed to address pressure ulcer development in hospitalized patients, HAPI’s national prevalence and treatment costs remain high. For example, approximately 2.5 million American patients in intensive care units annually develop pressure injuries that result in 60,000 deaths (Padula & Delarmente, 2019). The incidence rate of HAPIs in intensive care units varies from 14% to 42% (Anderson, 2020). Moreover, according to Padula and Delarmente (2019), the treatment cost for one pressure injury ranges from $500 to $70,000 because HAPIs lead to more extended hospital stays. For instance, the length of stay of patients with HAPI can increase to 14 days that causes a tremendous disturbance to patients’ physical and emotional well-being (Ricci et al., 2017).
Therefore, finding an effective intervention is critical for resolving multiple issues associated with HAPI. Indeed, the exploration of this topic started in the nineteenth century, and the first intervention to prevent HAPIs was developed by Browning (Mansfield et al., 2019). Still, research in this field was started a long time ago, but the approach that would eliminate a high HAPI prevalence problem has not been described yet.
Since various risk factors contribute to the development of HAPIs, introducing the pressure injury prevention bundle can address several issues simultaneously. The risk factors associated with the formation of pressure ulcers include older age, reduced mobility, poor nutrition, dehydration, reduced tissue perfusion, oxygenation, and medical devices placement (Romanelli et al., 2018). It appears that many intensive care unit patients have an increased likelihood of the development of HAPIs.
Therefore, implementing the prevention bundle, a combined scheme of standardized methods that target different aspects of the pressure ulcers issue, can minimize risks and reduce the HAPI incidence rate (Rivera et al., 2020). The elements of this method may vary between authors; however, numerous US-based quality-improvement clinical studies demonstrated the effectiveness of this approach regardless of the number of components in the bundle (Lin et al., 2020). Therefore, this evidence-based practice will be presented and utilized in this project to attain lower HAPI prevalence in the intervention site.
The primary function of the pressure injury prevention bundle is to recognize pressure ulcers in high-risk patients and introduce appropriate measures to prevent further progression of the damage. For example, the SAFER bundle, which stands for skin emollients, head-to-toe assessment, float heels, early pressure identification, and repositioning, allowed North Memorial Nursing Service to reach the drop of HAPI prevalence from 15% to 2% (Anderson, 2020). Other types of the bundle include skin assessment, surface support, incontinence, nutrition, and mobility (Romanelli et al., 2018).
The bundle approach that will be used in this project was developed by Rivera et al. (2020), whose methodology is based on assigning intervention depending on the severity of tissue damage. Specifically, patients with superficial HAPIs can receive a standard treatment plan, while those with deep pressure ulcers should get high-risk intervention (Rivera et al., 2020). The effectiveness of this approach was tested in an 11-bed critical care unit in one of the hospitals in New York City (Rivera et al., 2020). The results of the study demonstrated a seven-fold decrease in HAPI incidence in this department.
Since the DPI project focuses on an actual problem, it should follow a specific structure to ensure that it offers a scientific meaning. Thus, Chapter 1 presents general details, including background information, problems statement, the project’s purpose, clinical question, and explanation of how the work advances scientific knowledge. Chapter 1 also presents data regarding the project significance, the rationale for choosing a specific methodology and a project design, definitions of terms, key assumptions, limitations, delimitations, and the summary.
Simultaneously, Chapter 2 presents the literature review on the topic. This chapter also offers detailed information regarding the topic’s background and comments on the theoretical foundations of the DPI project, focusing on nursing and change theories. In turn, Chapter 3 focuses on the project’s methodology, considering population, instrumentation, validity, reliability, data collection, data analysis, and other relevant issues. Chapter 4 will present the graphic and written description of the results. Chapter 5 outlines the assessment of the findings and discusses them.
Background of the Project
Pressure injuries are not a new issue in the healthcare industry, which denotes that they can be considered from a historical perspective. According to the World Health Organization (WHO) (2008), this issue’s prevalence is similar in different nations, including 10% in the USA, 11% in Germany, 12% in Sweden, and 13% in Israel (p. 45). The Joint Commission (2016) defines pressure injury as localized skin and tissue damage related to exposure to a medical device. Ricci et al. (2017) stipulate that the pressure ulcer prevalence was slightly lower than 15% in 1999, while the 2009 International Pressure Ulcer Prevalence Survey revealed similar results. Li et al. (2020) argue that the HAPI prevalence is 12.8%, while the incidence rate is “5.4 per 10,000 patient-day” (p. 2). These statistical data reveal a challenging situation in health care and Padula et al. (2019) state that pressure injuries “affect over 2.5 million individuals resulting in 60,000 deaths” (p. 132). This information demonstrates that pressure injuries continue to be a problem in the healthcare industry.
The issue is differently represented in the community under investigation. According to the New York State Department of Health (2017), the community has overall an effective response to the problem because the state average HAPI prevalence is 0.1% (para. 4). However, there exist individual facilities where the incidence is 5%, 6%, and even 30% (New York State Department of Health, 2017, para. 5). As for the project site, it has a rate of 14%. This information demonstrates that the local data are slightly different from global data, but it highlights the necessity to address the problem.
Problem Statement
This project will focus on the 13-bed MICU in urban New York, where the number of patients with HAPIs was found to be higher than the national average. Specifically, this unit reports the prevalence of pressure ulcers of 14%, which means that every tenth patient in MICU will develop HAPI. Furthermore, MICU is the primary facility that admits HAPI cases; thus, 55% of all pressure injuries in the hospital are found in this unit. The average age of MICU patients is 68, which is a significant risk factor for HAPI. Moreover, most patients in the department are critically ill, placing them in a high-risk group for pressure injuries development. It appears that addressing this problem is vital to improving patient outcomes in MICU.
However, it is unknown if or to what degree the implementation PIP bundle would impact the HAPI incidence compared to current practice among the critical care unit population in a 13-bed unit in urban New York. Even though this problem statement focuses on a single medical establishment, it does not mean that the project’s need is limited to this facility. Therefore, it is essential to determine whether utilizing the PIP Bundle can lead to better health outcomes.
Wang et al. (2020) acknowledge that the HAPI risk depends on age and the length of hospital stay. It denotes that the risk of suffering from a pressure injury is higher for adults and positively connected to a person’s age. Simultaneously, the studies by Hultin et al. (2019), Latimer et al. (2019), Mäki-Turja-Rostedt, Stolt, Leino-Kilpi, and Haavisto (2019), and many others also focus on HAPIs among older patients. This information indicates that the DPI project focuses on older hospitalized individuals from a single healthcare unit since they represent the broad population significantly affected by the problem. The rationale behind this claim is that these people are under the influence of specific HAPI risk factors.
The DPI project can contribute to solving the problem because it offers to find a practical solution of how to protect the identified population from HAPIs. Since this study field provides mixed findings regarding the PIP Bundle, it is reasonable to conduct a quality improvement project that can offer precise results. If the DPI project reveals that the PIP bundle leads to significantly better outcomes, the healthcare industry can obtain a practical guideline to reduce the HAPI incidence. If the intervention does not lead to improvement, it will be necessary to look for other quality improvement measures. In this case, it can be reasonable to utilize a different methodological approach to studying the issue.
Purpose of the Project
The purpose of this quantitative quasi-experimental project is to determine if or to what degree the implementation of the PIP Bundle would impact the HAPI incidence when compared to current practice among critical care patients in a 13-bed unit in urban New York. The independent variable, PIP Bundle, will be defined as the standard and high-risk pressure injury prevention bundles. The dependent variable, a HAPI incidence rate, will be measured by the number of patients who develop this condition during a hospital stay. The project site collects data about pressure injuries in its electronic health records (EHRs) that can be used for this project, and the facility indicates that HAPIs are a problem. It denotes that the given healthcare unit frequently deals with pressure ulcers among its patients, meaning that it will benefit from quality improvement.
For this purpose, the wound care team will access these EHRs to identify whether a patient experiences a pressure ulcer. It is expected that the implementation of the independent variable can result in the reduced spread of the dependent one among the population under investigation. The project’s purpose is aligned with and builds on the problem statement above because the two focus on the same issues. This requirement is necessary to ensure that the DPI project is consistent.
It is possible to mention that the DPI project will offer an essential contribution to the field. The rationale behind this statement is that multiple scholarly articles admit that the older population significantly suffers from HAPIs. They typically have deteriorated health conditions that make them experience pressure ulcers when they are hospitalized. Extended periods of hospital stay denote that patients spend much time in a sitting or lying position. Consequently, their skin is subject to constant pressure that, in turn, results in the occurrence of HAPIs. This situation describes that the DPI project will address an essential issue that creates some challenges for a specific population. This statement is based on the issue that a few healthcare facilities in New York suffer from increased HAPI incidence (New York State Department of Health, 2017). That is why the DPI project tries to address this adverse state of affairs, which can provide the whole healthcare industry with noticeable improvement. Finally, it is worth admitting that the cost of pressure ulcer care will not be an aspect of the project because the intervention can be implemented free of charge.
Clinical Question
It is challenging to predict what bundle methodology should be introduced in MICU and what outcomes will be achieved. Although the prevention bundle was proven to diminish the HAPI incidence rate in many clinical studies, the statistical significance of their results could not be obtained in some cases (Lin et al., 2020). Therefore, it is unknown if the issue of high HAPI prevalence in MICU will be resolved with the chosen approach.
The question guiding this project is: To what degree does the implementation of the PIP bundle impact the HAPI incidence compared to current practice among critical care patients in a 13-bed unit in urban New York over four weeks? The question also reveals that the project seeks to identify whether the use PIP bundle, the independent variable, is sufficient to reduce the HAPI incidence, the dependent variable. That is why the DPI project attempts to conduct a specific quasi-experimental study to answer this question.
This discussion demonstrates that the DPI project tries to identify the effectiveness of the PIP bundle. The clinical question reveals that it is possible to cope with this task if the project deals with specific variables. Potential reduction in the HAPI incidence will be measured according to the medical establishment’s EHRs. However, it is necessary to state that the project should focus on a specific sample size to limit its scope. Furthermore, only adult critical care patients will be included in this study. The rationale behind this selection is that critical care patients are more prone to multiple risk factors that contribute to the spread of pressure ulcers (Mervis & Phillips, 2019). That is why it is essential to determine whether the PIP bundle leads to the expected positive outcomes among critical care patients.
Advancing Scientific Knowledge
Scientific evidence demonstrates that the problem under consideration is consistent. Ricci et al. (2017) stipulate that the pressure ulcer prevalence was slightly lower than 15% in 1999, while the 2009 International Pressure Ulcer Prevalence Survey revealed approximately the same results. Even though the issue created fundamental problems for the whole medical industry, no improvement attempts could generate the required outcomes. As for the current state of affairs, Li et al. (2020) argue that the HAPI prevalence is 12.8%, while the incidence rate is “5.4 per 10,000 patient-day” (p. 2). These statistical data reveal a challenging situation in health care, and Padula et al. (2019) support this claim stating that pressure injuries “affect over 2.5 million individuals resulting in 60,000 deaths” (p. 132). This information demonstrates that pressure injuries continue to be a problem in the healthcare industry. Consequently, there is a gap in care because the current practice is insufficient to reduce HAPI incidence and prevalence.
The DPI project will advance scientific knowledge in the sphere of addressing pressure injuries among hospitalized patients because evidence-based practice addresses the gap. Many scholarly studies, including those by Hultin et al. (2019), Latimer et al. (2019), and others, comment on the effectiveness of turning and repositioning patients every two hours. For example, Courvoisier et al. (2018) and Pechlivanoglou et al. (2018) admit that 2- and 3-hourly interventions are more effective. Simultaneously, Chew et al. (2018), Sharp et al. (2019), and others report no differences between various turning and repositioning intervals. These data reveal the existing need in the current literature because multiple studies offer contradictory results regarding the intervention under consideration. The literature demonstrates that turning and repositioning is an evidence-based practice that addresses the identified gap.
Human caring nursing theory (Watson, 2018) is used in this DPI project to identify how 2-hourly turning and repositioning can be associated with reduced HAPI incidence. Jean Watson (2018) proposed this theoretical framework by highlighting how to improve positive outcomes during human-to-human caring moments. She stipulates that patients cannot be separated from the healthcare workforce, implying that a change occurs through nurses. This information demonstrates that the theory will drive the intervention because it denotes healthcare workers should make hospitalized patients turn and reposition.
The study by Kennerly and Yap (2018) demonstrates that the theory can be applied in evidence-based practice projects. The project can advance this theory by demonstrating whether its application leads to positive outcomes when applied to 2-hourly turning and repositioning and the HAPI incidence. If positive results are found, it will be possible to state that it is reasonable to rely on this theoretical framework to combat the issue of pressure ulcers. The project also adds to explaining what role healthcare professionals play in combatting pressure injuries.
Significance of the Project
High healthcare costs are a significant problem in the United States. Prolonged hospital stays due to the development of pressure injuries in intensive care unit patients complicate this issue further. For example, treatment of superficial pressure ulcers may cost about $500, while the price of more advanced HAPIs can rise to $70,000 (Padula & Delarmente, 2019). The fact that every tenth patient in MICU in urban New York hospital requires secondary intervention that may cost higher than the primary treatment demands introducing preventive measures to minimize these expenses. In addition to economic benefit, patient outcomes and satisfaction will increase because their quality of life will be improved, allowing them to have shorter hospitalizations and return to their families early. Many clinical trials achieved a significant reduction in the HAPI incidence rate. For example, a quasi-experimental clinical study by Anderson (2018) reached a seven-fold drop in the prevalence of pressure injuries. Similarly, this project aims to utilize this study design to determine how effective the selected scheme of pressure injury prevention bundle will be in the 13-bed MICU.
The problem of pressure injuries is widespread in the medical industry. Padula et al. (2019) argue that this health condition affects more than 2.5 million people. Padula and Pronovost (2018) also admit that HAPIs result in 60,000 deaths in the USA annually, and their costs are estimated at $9-$11 billion. Simultaneously, Li et al. (2020) argue that the HAPI prevalence is 12.8%, while the incidence rate is “5.4 per 10,000 patient-day” (p. 2). The WHO (2008) states that this issue’s prevalence is similar in different nations, including 10% in the USA, 11% in Germany, 12% in Sweden, and 13% in Israel (p. 45). These data indicate that a significant part of the US population is subject to this health condition. Simultaneously, the project site reports that it suffers from an 11% prevalence that refers to the incidence of 10 HAPIs per 100 patients. That is why there is a necessity to find a practical solution to minimize the spread of the issue and protect individual health.
The information above makes it predictable that the project is not unique in addressing the topic. The studies by Atkinson and Cullum (2018), Gaspar, Peralta, Marques, Budri, and de Matos (2019), and Mäki-Turja-Rostedt et al. (2019) also focus on the use of turning and repositioning to prevent pressure injuries. These studies represent an evidence-based practice approach to the problem. Still, there is a gap in the literature because multiple articles offer mixed findings regarding the effectiveness of the proposed intervention. Since the current literature comments on the possible efficacy of turning and repositioning approaches, the project aims at enriching knowledge. Since multiple studies offer conflicting findings regarding the proposed intervention’s effectiveness, this paper is an attempt to identify the actual effect of 2-hourly turning and repositioning. Consequently, the DPI project is significant since it addresses a sensitive topic in the healthcare industry and aims at generating unambiguous conclusions regarding the issue under investigation.
The DPI project completion is also significant for numerous stakeholders. Firstly, clinicians, nurses, and other healthcare professionals can witness essential benefits since the project offers an opportunity to advance the quality of care relating to older patients (Hultin et al., 2019; Latimer et al., 2019). While these people typically suffer from deteriorated health conditions, it is reasonable to provide them with improved care, and the project tries to cope with it. It is expected that the results will improve the clinical site practice because the project can reveal efficient, practical applications. Secondly, there is an evident connection between the project and improved public health. The rationale behind this statement is that the project can develop specific guidelines for healthcare professionals to ensure that patients are less subject to pressure injuries. Finally, the project can be beneficial for the whole healthcare industry. The financial impact is the key, and Padula and Pronovost (2018) admit the financial burden of this issue, meaning that its prevention can make the medical system more cost-effective. It denotes that the DPI project can effectively protect older hospitalized populations from pressure injuries.
Rationale for Methodology
A quantitative methodology is effective in addressing a clinical problem and answering a clinical question. The rationale behind this statement is that it relies on numerical data, and this approach is necessary to identify the incidence of a particular phenomenon. For that purpose, various statistical tests should be used, and Bell, Bryman, and Harley (2018) admit that this methodology applies some of them, including t-test, which increases the reliability of the obtained results. Creswell and Creswell (2018) explain that the main benefit of this approach is that it allows for conducting an experiment to collect and analyze the data. Simultaneously, Rutberg and Boukidis (2018) stipulate that a quantitative method is appropriate when answering a clinical question to achieve quality improvement. The articles by Aljezawi and Tubaishat (2018), Edger (2017), Sharp et al. (2019), and others rely on this method to identify the effectiveness of turning and repositioning interventions. One can admit that these and other researchers tend to rely on the given approach because it is suitable for identifying the connection between independent and dependent variables.
Simultaneously, it is reasonable to explain how this methodology answers the project’s clinical question and addresses the problem statement. The problem statement reveals that it is necessary to compare the effectiveness of two interventions, and the description above shows that a quantitative method is a suitable option to cope with the task. Simultaneously, the clinical question attempts to identify a measure of improvement, and the selected methodology runs statistical tests to find this answer.
Nature of the Project Design
The DPI project uses a quasi-experimental design to answer the clinical question. The reason for selecting this approach is the necessity of applying the intervention (PIP Bundle) and identifying whether it leads to improved outcomes (reduced HAPI incidence). Thus, the given design is relevant because Rutberg and Boukidis (2018) state that it allows for assessing the intervention’s effectiveness for quasi-experimental and comparison groups.
Simultaneously, it is reasonable to contrast the design to the correlational and experimental ones. Siedlecki (2020) also admits that case studies, descriptive, and correlational designs are not appropriate since they are less practical than the selected approach. On the one hand, a correlational design is inappropriate since it does not imply using a controlled intervention. On the other hand, an experimental design is not suitable since it implies randomization, which would make the project more time and resource-consuming. Thus, it is necessary to stipulate that the quasi-experimental design is ideally aligned with the quantitative methodology.
It is reasonable to provide a detailed explanation of the project design. Since the project is the implementation of evidence-based practice (EBP), it follows a before and after design. Consequently, the project sample should be divided into two groups. The before group includes those patients who receive the standard of care that is turning and repositioning every four hours. As for the after group, it consists of those participants who are subject to 2-hourly turning and repositioning. The project implies that it is necessary to collect and analyze the data regarding the number of pressure injuries that developed in the two groups. This approach denotes that it is required to identify the HAPI incidence within each group and compare the obtained data to determine whether there is an improvement following the proposed intervention. An appropriate statistical test is necessary to identify whether the changes are statistically significant and directly connected to the intervention.
The discussion of the DPI project design should devote sufficient attention to data collection and work with the project variables. The dependent variable that is the intervention is the use of repositioning and turning every hour. This term stands for actions and efforts to make hospitalized patients change their postural positions. Nurses should ensure that the project participants follow the prescribed one-hour schedule. The independent variable refers to a HAPI incidence rate measured by focusing on the number of patients who develop pressure injuries during their hospital stay. The data for the independent variable is collected by analyzing EHRs after the end of the intervention process. These data may only be accessed after the facility under investigation issues corresponding permission. This discussion proves the statement by Rutberg and Boukidis (2018) that the quasi-experimental design is suitable for this DPI project. Thus, one can stipulate that the selected project design is appropriate to answer the clinical question.
Definition of Terms
The following terms are operationally defined in lay words and in the context in which they appear in the paper.
Pressure Injury Prevention Bundle. This approach allows clinicians to have guidance for the assessment and monitoring of intensive care unit patients. This term refers to the plan of care that was developed to prevent the development of pressure injuries in patients at risk (Romanelli et al., 2018). The prevention bundle elements may vary between authors, but the overall goal of all methods is to prevent further complications of HAPI.
Turning (i.e., Repositioning). Even though these are separate words, they are often used interchangeably in scholarly literature. That is why their meaning is the process when individuals move or change their position while sitting or lying. There exist two approaches to promoting turning and repositioning in the healthcare industry. On the one hand, Schutt, Tarver, and Pezzani (2018) indicate that self-turns and rolls are an effective strategy for hospitalized patients to avoid pressure ulcers. On the other hand, Woodhouse, Worsley, Voegeli, Schoonhoven, and Bader (2019) state that medical professionals can turn and reposition individuals. This term represents the independent variable of the given DPI project.
Pressure Ulcers (HAPIs). This term denotes “areas of localized injury to the skin and underlying tissue, usually over a bony prominence, as a result of pressure, or pressure in combination with shear” (Li et al., 2020, p. 2). This health condition is widespread, affecting people’s psychological and physiological well-being. The HAPI incidence is the dependent variable of the given project.
Assumptions, Limitations, Delimitations
The following assumptions are present in the given DPI project:
- It is assumed that the project participants do not create any treatment barriers and diligently follow the PIP bundle offered to them. This idea is necessary since it implies that changes in the HAPI incidence, if any, are directly related to the intervention, not external processes.
- Another assumption denotes that the DPI project will identify the positive connection between providing a PIP bundle and the decreased HAPI incidence. This statement implies that the project aims at arriving at the conclusion that utilizing the PIP bundle is an effective pressure injury prevention intervention.
- One more assumption is that the healthcare facility correctly enters the data on patient’s pressure injuries in their EHRs. This condition is necessary because the project relies on EHRs to identify the HAPI incidence.
The following limitations are found in the project:
- Time constraints can be considered an essential limitation of the project. Since the project covers four weeks, it fails to assess the long-term effect of the proposed intervention.
- Another limitation is a small sample size because the project focuses on patients from a single medical facility in urban New York. That is why it can be impossible to generalize the obtained results and determine whether the proposed intervention can be effective for the larger population.
- One more limitation is that the project depends on how accurately and diligently the facility approaches its reporting system. It relates to the fact that if the healthcare unit fails to mention in its EHRs that some patients experience pressure ulcers, the project’s results will suffer.
The following delimitations are found in the project:
- The project is delimited to a 13-bed critical care unit in urban New York. This delimitation is necessary because critical care patients are more subjected to pressure injuries due to poor tissue perfusion or hemodynamic instability.
- Another delimitation is that the project chooses a nursing theory by Jean Watson (2018) to ensure that the project has some theoretical support.
It is reasonable to mention that the limitations above can be overcome in future projects. For future papers, it is necessary to conduct a more extensive project that will include more participants who will be under investigation for a more extended period. Simultaneously, it will be reasonable for researchers to have greater control over the future project by participating in reporting activities to minimize its dependence on a facility.
Summary and Organization of the Remainder of the Project
Chapter 1 has presented basic information regarding the DPI project. Padula et al. (2019) explain that HAPIs are a significant problem in the healthcare industry, meaning that a practical intervention is necessary to address the issue. Chapter 1 has also formulated the problem statement, the purpose of the project, and the clinical question. Evidence from scholarly sources demonstrates that the project can advance scientific knowledge because the existing literature offers conflicting results of using turning and repositioning (Courvoisier et al., 2018; Sharp et al., 2019). Thus, the project is significant since it aims at addressing this gap and providing multiple stakeholders, including patients, healthcare professionals, and the whole medical facilities, with essential benefits.
Chapter 1 also comments on the methodological aspect of the project. The intervention for reducing HAPI prevalence was presented in this chapter. Specifically, the background knowledge about the pressure injury prevention bundle developed by Rivera et al. (2020) and some other variations of this approach are discussed in chapter 1. Creswell and Creswell (2018) justify using a quantitative approach, while Rutberg and Boukidis (2018) explain that it is reasonable to use a quasi-experimental design. Then, the key terms are defined to ensure that anyone reading the DPI project can accurately understand the concepts under discussion. The project assumptions, limitations, and delimitations have also been discussed in detail, while specific comments are offered on how to overcome these limitations in a future project.
At this point, it is also appropriate to present the organization of the remainder of the project. Chapter 2 will overview the current literature on the PIP bundle and whether this intervention effectively prevents pressure injuries. Chapter 3 will present a detailed description of the project methods and procedures, commenting on the sample, data collection, data analysis, and other methodological affairs. Finally, Chapter 4 will introduce a graphic summary of the project results, while their discussion and interpretation will be offered in Chapter 5.
Literature Review
A hospital-acquired pressure injury is a preventable event that often happens in the intensive care unit. A pressure injury is localized skin and tissue damage caused by intense and continuous pressure (Anderson, 2020). The risk factors for developing healthcare-acquired pressure injuries are immobility, altered mental status, and advanced age (Frank et al., 2017). This review aims to uncover the importance of implementing a pressure injury prevention bundle in reducing the prevalence of pressure ulcers in critical care units.
Pressure Injuries (PIs) refers to local injuries to the subcutaneous tissue or the skin, and they are usually are experienced over bonny prominences. They are caused by pressure, and it sometimes comes with shear forces. Hospital-acquired pressure injuries (HAPIs) usually increase the medical burden, workload of nurses, as well as length of hospital stay (Gaspar et al., 2019). It tends to lower patient’s health-related quality of life (HRQOL). They increase mortality and cause diverse medical disputes affecting patients’ experience. Many risks factors exist for PI, particularly for critical-care patients, including poor perfusion, older age, as well as change in mobility. Critical care patients are exposed to a greater risk of developing PIs, implying that it is important to establish effective measures to improve the safety of patients in intensive care units (ICUs). The bundle approach is a care standardizing process meant to promote patient outcomes. It argued that its success depends on various factors, including the involvement of key stakeholders, audits and feedback, and the motivation of the pressure injury prevention teams.
Patients in critical care units (CCUs) are exposed to a risk of developing HAPIs. This project will support the use of a pressure injury prevention (PIP) bundle to reduce incidences of HAPIs in an adult setting. It will focus on enhancing the identification of the best bundle implementation and PIP practices (Gaspar et al., 2019). This will influence the standardization of the HAPI prevention process and lower incidences of HAPI incidences. Implementation of the project will require leadership and staff involvement to hinder HAPIs. The literature review will be organized into various sections, namely introduction, theoretical foundation, review of the literature, and summary.
The theoretical framework will discuss Kurt Lewin’s (1951) change management theory to support the analysis of forces and subsequent balancing of the change plan. The theory will offer an effective framework for the preventive bundle. Lewin’s Change Theory entails a three-step change model, and it is effective in supporting the implementation of interventions to enhance the achievement of desirable changes in nursing. The review of the literature will be supported by four main themes and several sub-themes. The main themes will be turning, repositioning, and offloading, pressure injury prevention bundle: high-risk interventions, pressure injury prevention bundle: standard risk interventions, and hospital-acquired pressure injuries/ulcers (HAPIs/HAPUs).
The DPI project should undertake a thorough literature review to analyze the existing information. It is reasonable to search professional databases to find credible and timely literature on the topic. That is why a suitable approach is to use Google Scholar since this service provides simultaneous access to multiple resources, including PubMed, Cochrane, EBSCO, BMJ, CINAHL, and others. The following keywords and their various combinations are used to identify the required sources of information: pressure injuries, pressure injury prevention bundle, interventions related to pressure injuries, risk factors, and incidence related to pressure injuries. The search results are limited to the studies that are published not earlier than in 2017 to ensure that the DPI project deals with the most recent literature. The identified articles are included in the project based on their abstracts. The articles are included if they are available in full text and peer-reviewed. As a result, 90 studies were retrieved, while a set of 50 credible and reliable studies are selected for this literature review.
Pressure injuries affect multiple patients, and it is impossible to deny that some improvements are needed. Ricci, Bayer, and Orgill (2017) admit that “the overall pressure injury prevalence rate described in 1999 for acute care facilities was 14.8 percent” (p. 275e). Simultaneously, the 2009 International Pressure Ulcer Prevalence Survey revealed approximately the same results irrespective of some improvement measures (Ricci et al., 2017). Simultaneously, Li et al. (2020) indicate that the current HAPU prevalence is 12.8%, while the incidence rate is “5.4 per 10,000 patient-day” (p. 2). These findings demonstrate that a gap exists because no significant improvements have occurred over more than 20 years in the sphere of addressing pressure injuries.
Theoretical Foundations
Human caring nursing theory is used in this DPI project to identify how PIP bundle can be associated with reduced HAPI incidence. Jean Watson (2018) proposed this theoretical framework by highlighting how to improve positive outcomes during human-to-human caring moments. Wei and Watson (2019) also indicate that the theory relies on practice, research, and theory-based education to ensure that any proposed intervention is suitable and can help patients achieve better health outcomes. This theory denotes that successful results can only be achieved if a medical practice is backed theoretically.
In addition to that, the DPI project focuses on a specific change theory. It refers to Kurt Lewin’s (1951) change management theory that is typically used for numerous quality improvement projects. This framework implies that patients change their behavior under the influence of driving or positive forces that affect individuals from outside (Lewin, 1951). This information suggests that it is necessary to provide patients with external support to ensure that they can overcome some challenges.
The change model above implies that the DPI project will rely on specific steps to measure the variables. Firstly, it is necessary to improve patients’ knowledge about the problem and its possible solutions. In this case, the findings from Ricci et al. (2017), Li et al. (2020), Courvoisier et al. (2018), and others are helpful. This information justifies the use of PIP bundle and HAPU incidence as the project variables. Secondly, it is reasonable to implement a change by subjecting patients to specific interventions. One can suppose that applying the chosen change theory is appropriate to answer the identified clinical question.
Review of the Literature
The literature review collects and analyzes findings from 50 credible and reliable sources. It is worth admitting that most of these sources were published within the last five years, which indicates that the DPI project relies on timely data. Reliable sources will be consulted to ensure the provision of valid and relevant information. The objective will be to survey the available literature on pressure injury prevention bundles and offer a synthesis of the information. It will offer a critical analysis by focusing on the identification of the existing gaps in the current knowledge. This will be done by evaluating the existing limitations of theories as well as consider different views of authors. The literature review will show that the research is valid and add beneficial information to the available knowledge. This implies that it will summarize and integrate known information regarding the implementation of pressure injury prevention bundles in critical care. It will evaluate strategies adopted to reduce hospital-acquired pressure injuries and promote patient safety.
The purpose of the literature review is to enhance the standardization of HAPI prevention strategies in an adult setting. It encourages the establishment of an interdisciplinary team including nurses, managers, patient care associations, and respiratory therapists. It will support the development of a comprehensive approach and promote the engagement of stakeholders, sustainability, adherence, and adoption. Evaluating diverse studies will enhance the understanding of the development, implementation, evaluation, and monitoring of the pressure injury prevention bundle (Gaspar et al., 2019). It will assess evidence-based practices to explain how existing challenges can be eliminated. Moreover, the literature will identify gaps in the existing research and suggest areas where further studies need to be conducted. The literature will build an argument entailing how the development of the research question while explaining the current models, topics, and theories. It will enable the reader to understand the importance and relevance of the project.
Hospital-Acquired Pressure Injuries/Ulcers (HAPIs/HAPUs)
Hospital-acquired pressure injury (HAPI) affects patient care since it is associated with deleterious consequences for the healthcare system and patient. It is vital to reduce incidences of HAPI, particularly in the ICU, since it presents many problems. It has a major financial implication, with its cost extending beyond $2,000 per PI. The involved cost and associated human suffering explaining the dire need to establish effective preventive strategies (Gaspar et al., 2019). Moreover, the scope of the problem is high and involves multiple levels. Rivera et al. (2020) revealed that at least one million people develop PI annually in the U.S. The study also indicated that 2.3 million patients in acute care facilities develop the condition where more than 60,000 lose their life due to related complications (Gaspar et al., 2019). High incidences can influence the affected organization to lose reputation and eventually face financial challenges. The National Quality Forum (NQF) considers most of the HAPIs preventable.
The application of a care bundle can help hinder PIs even better than clinical guidelines. They entail a set of nursing interventions for a given individual or class of patient to promote healthcare outcomes. The approach is beneficial since it is based on the best evidence, and it is associated with many benefits to patients. There exists an association between the best evidence and bundle approach since it promotes positive clinical outcomes (Green et al., 2018). However, it is faced with challenges such as the severity of the patient’s illness and the complexity of the ICU environment. It is necessary to evaluate the implementation compliance when using the care bundle. It is difficult to realize the benefits of evidence-based practical intervention without considering intervention guidelines. This implies that it is not possible to maximize the benefits obtained from the evidence-based practical intervention in case teamwork and effective communication are ignored (Gaspar et al., 2019). Understanding the quality of the bundle as well as its implementation requires the determination of the effectiveness of the prevention approach, particularly its usefulness during clinical setting trials. Compliance with care bundles can improve interventions and help achieve the desired outcome.
Risk Factors and Incidence Rates
Patients in the critical setting are exposed to higher risks and incidence rates for the development of HAPIs/HAPUs. In this regard, it is crucial to establish a clear understanding of this phenomenon. Chadboyer et al. (2018) review this issue at length within the framework of a systematic review. The purpose of their research was to examine the problem of pressure ulcers that emerge as a result of clinical treatment in terms of scale and scope. The conclusions are made based on the in-depth analysis of twenty-two studies that were reviewed and synthesized in alignment with the research questions. Chadboyer et al. (2018) report the cumulative incidence of HAPUs to be within the range of 10-26%. These numbers indicate that the matter at hand represents an issue of a serious magnitude. As for the location of the HAPUs, the systematic review indicates that most of them emerge on the patient’s sacrum, followed by the buttocks, heel, hips, ears, and shoulders (Chadboyer et al., 2018). Accordingly, pressure ulcers affect a considerable number of patients, causing moderate-to-severe discomfort in the fallout of prolonged care.
The problem of HAPIs is not unique to the United States or any other country. Li et al. (2020) explore the issue from a global perspective, utilizing the international experience to address their clinical question. More specifically, they aim to “quantify the prevalence and incidence of pressure injuries and the hospital-acquired pressure injuries rate in hospitalized adult patients” (Li et al., 2020, para. 2). In order to address the research purpose, the authors rely on the formats of systematic review and meta-analysis. The research sample comprises cross-sectional, observational, and longitudinal studies that report HAPUs among hospitalized adults. Based on the examination of forty-two relevant studies and a total sample of 2,579,049 patients, Li et al. (2020) report an incidence rate of 5.4 per 1,000 patient days. Most of the HAPU cases represent stages I and II of the condition (71,5% in total). From a geographical perspective, the analysis revealed a considerable level of heterogeneity, implying certain territorial correlations that are to be explored in subsequent examinations. This study highlights that the prevalence of HAPUs is a global healthcare concern, but its exact magnitude may vary across different settings.
Evidently, exploring the prevalence of pressure ulcers in the clinical setting per setting will not yield substantial improvements. Accordingly, Greenwood and McGinnis (2016) venture into the territory of the root cause determination. Their article aims to outline the primary avenues of HAPU’s development in acute care environments. The authors apply data analysis methods to process the findings obtained by the root cause analysis process implemented in the U.K. since 2010. The practical purpose of such research consists of identifying the key themes and learning points that can help develop meaningful solutions to the clinical issue in question. The research sample comprised thirty-two HAPU RCA’s that provided insight into the origins of the problem. According to Greenwood and McGinnis (2016), malnutrition becomes the primary root from which increased incidence rates of HAPUs in acute care stem. However, analysis suggests that patient pressure injuries rarely appear in the fallout of a single cause, becoming a product of a combination of factors. More specifically, the authors of the study refer to HAPU emergence as a “sequence of events” that leads to adverse consequences in terms of patients’ well-being. Ultimately, the understanding of the problem’s roots in specific contexts is a major step toward the provision of meaningful solutions.
A similar perspective was taken by the authors of the next study, who explored the risk factors contributing to the development of HAPU’s in the clinical setting. Dreyfus et al. (2017) utilized U.S.-based data in order to address their clinical question. It revolved around identifying and categorizing the primary predictors of pressure injuries that occur during a patient’s prolonged stay at a facility. The authors refer to HAPUs as a major “societal burden” that can be effectively addressed and prevented if major underlying causes are correctly determined. Dreyfus et al. (2017) investigated 47,365 HAPU cases among 16,967,687 patients with a cumulative incidence of 0.28%. As per the findings, the prior incidence of pressure injuries is the most important predictor of future cases, along with a history of diabetic foot ulcers. In addition, the authors concur with the findings provided by Greenwood and McGinnis (2016), placing malnutrition among the most important causes of HAPUs. The impact of the condition is equally assessed, as authors report an increased duration of stay and elevated hospitalization costs in the case of pressure injuries.
As can be inferred from the current body of knowledge, predictors and determinants of HAPU’s form an area of intense interest for researchers across the globe. Kayser et al. (2019) conduct their study along similar lines, venturing into the underlying issue territory. In terms of the clinical question, the authors of this article explore the differences between risk factors associated with a superficial and severe case of HAPU’s. As per the study’s design, 216,626 complete patient datasets from acute care hospitals in the United States were analyzed. Having generated the annual linear trendlines, Kayser et al. (2019) performed two logistic regressions to examine the risk factors. The accumulated risk factor list comprised “increased age, male gender, unable to self-ambulate, all types of incontinence, additional linen layers, longer durations of stay, and being in an intensive care unit” (Kayser et al., 2019, p. 46). In addition, a U-shaped relationship between HAPU risks and body mass index was observed. In this context, both extremely low and high BMIs were associated with increased pressure injury risks. Thus, this study introduces physical parameters that represent specific risk groups to be addressed in further interventions.
Overall, hospital-acquired pressure injuries have a long history of a negative influence on the functioning of the healthcare system. This issue is global in nature, as institutions across the world face its adverse implications. However, as can be inferred from the current body of knowledge, the exact incidence rate of the HAPUs is inconsistent across various settings. In addition, the vast majority of cases represent Stages I and II of the condition, accounting for over 70% of all cases. As per the academic consensus, HAPUs originate from various factors that usually act in a combination. More specifically, prior cases of hospital-acquired pressure injuries make a patient subject to new instances of the condition in the future. In addition, aside from previous cases, malnutrition remains a prevalent predictor of HAPUs in the clinical environment. A considerable part of the contemporary research is aimed at the identification of key determinants that aggravate the issue. Through such studies, the system acquired a deeper understanding of these predictors and developed fitting solutions that address them effectively.
Patients with Specific Health Conditions
As can be inferred from the prior discussion, a number of underlying conditions can aggravate the development of HAPIs. Typically, this health issue is the most acute for individuals who spend much time in prone or sitting positions. However, other factors can facilitate the emergence of pressure injuries, prompting scholars to seek specialized methods for such particular cases. Thus, it is reasonable to identify research pieces that would make it clear whether PIP bundle is helpful for people with particular health conditions.
Cancer patients form one of the most vulnerable clinical groups in terms of both physical and moral aspects. Aljezawi and Tubaishat (2018) attempt to determine whether turning and repositioning are effective for cancer patients. A multicenter, cross-sectional prevalence study of 110 patients used a quantitative methodology to analyze the impact of 2-hourly repositioning on protecting such individuals from the health issue under analysis. The scholars conclude that irrespective of short frequency, this intervention does not guarantee that pressure injuries will not develop in cancer patients.
In addition, cardiovascular conditions may entail serious complications in stressful environments. Chitambira and Evans (2018) assessed the effect of repositioning for stroke patients with pusher syndrome and using a quality improvement initiative with 140 adults. The researchers draw attention to 2-hourly repositioning and placing of pillows. This article supports the claim that repositioning becomes more effective when it is used together with an additional intervention. Since the study focuses on a short intervention period, the authors highlight the necessity to organize further research on this topic.
As pressure injuries affect the skin tissue, corresponding health issues may also aggravate the development of this condition. Gray and Giuliano (2018) reveal that there is a robust correlation between pressure injuries and incontinence-associated dermatitis (IAD). A descriptive and correlational analysis of 5,342 adults demonstrates that an increased HAPU prevalence is found when it comes to focusing on IAD patients. The authors highlight that traditional prevention measures, including repositioning and turning, are not sufficient to protect the population from the given health condition. Thus, another argument in favor of a combined approach is made.
However, the range of underlying conditions is not limited to oncology, skin diseases, or cardiovascular issues. Mussa et al. (2018) focus on pressure injuries among patients with an endotracheal tube (ETT). A retrospective, pre-post intervention study indicates that a more frequent repositioning leads to some improvements, but they are not statistically significant. The authors prove it by analyzing data of 61 members from the pre-intervention group and 81 individuals from the post-intervention group. This finding demonstrates that it is not possible to rely on repositioning and turning exclusively to protect patients with ETTs from HAPUs.
The damage to a patient’s spine is a serious matter per se, limiting the mobility of a person. Eren, DeLuca, and Kirshblum (2020) consider what results turning and repositioning offer to patients with spinal cord injury. The authors do not implement any interventions but interview such individuals regarding whether they rely on the intervention. The findings demonstrate that almost half of the 86 respondents fail to turn regularly, irrespective of the fact that they are aware of this action. That is why it is not surprising that patients with spinal cord injury are subject to HAPUs.
This subtheme has a particular meaning for the entire project. Firstly, it proves that pressure injuries are a widespread problem that requires specific interventions. Secondly, the subtheme has revealed that individuals with particular health conditions are more subject to suffering from the given issue because they spend much time in sitting and prone positions. It indicates that turning and repositioning can only be effective for patients who do not suffer from additional issues.
HAPUs Impact on the Healthcare System
The elevated incidence rates of HAPUs form an area of concern for all parties involved in the delivery of medical services. In this regard, healthcare organizations equally sustain considerable damage, primarily in the financial domain. Padula and Delarmente (2019) extend this discussion even further, attempting to evaluate the national burden of hospital-acquired pressure injuries in the United States. In order to address the research question, the authors of the research rely on a Markov simulation. Through this method, they estimate the costs of staged HAPU’s that emerge during hospitalization from a medical organization’s point of view. As per the simulation’s results, the annual HAPU costs for the U.S. healthcare system exceed $26.8 billion, which is a colossal amount. Moreover, the distribution of the costs is not proportionate, as nearly 60% of the amount is a condition by the less frequent Stage III and Stage IV cases of pressure injuries. Therefore, the prevalence of HAPU’s undermines the financial aspect of the system, impeding the quality development of hospital units. In this context, significant progress can be made through the prevention of advanced-stage pressure injuries, alleviating the economic burden on organizations.
The immense economic impact of hospital-acquired pressure ulcers remains a matter of increased concern for the system’s management. Lim and Ang (2017) investigate this aspect of the problem within their research. The clinical report is based on the experience of a tertiary hospital in Singapore, thus contributing to the international dimension of the discussion. The clinical questions are presented from the managerial perspective, aiming at reducing the operational costs of healthcare organizations. The authors rely on the famous assumption, stating that the prevention of a problem is widely recognized as more effective than its treatment. In this regard, healthcare organizations are encouraged to pursue new avenues of reducing the incidence rates of HAPU’s like a phenomenon. These ideas align with the ongoing trends within the academic community, as researchers investigate the root causes of pressure injuries in order to develop stronger interventions. The examination by Lim and Ang (2017) reveals that HAPUs are a major stressor for hospitals, depleting their finite resources through prolonged stays, patient dissatisfaction, and corresponding expenses. Therefore, the impact of HAPUs on healthcare organizations is concerning, thus justifying the need for effective interventions.
As a matter of fact, the utilization of the international experience in the discussed context appears relevant and necessary. The problem of HAPUs is global in nature, making it necessary to synthesize and implement the world’s best practices into intervention projects. Han et al. (2019) follow the data obtained through practical observations and analyses in a South Korean hospital with increased HAPU incidence rates. The clinical question was whether these conditions affected the key parameters of a healthcare organization’s performance. More specifically, the authors of the study associate HAPU’s with a strong negative impact on the patient’s health. The sample of 1,000 patients was compared with a 4,000-person control group. The results indicate that advanced HAPUs are associated with increased mortality rates, putting additional pressure on patients and medical units. In addition, the average duration of stay for the patients who develop this condition is longer, leading to higher healthcare costs and financial burdens. Finally, the emergence of HAPUs is a serious predictor of readmission, which, in turn, equally undermines the performance of a medical organization. Therefore, all parties involved in the clinical procedure will benefit from effective interventions aimed at the prevention of hospital-acquired pressure injuries.
Ultimately, the information presented in this section confirms the multi-faceted adverse impact of HAPUs on the functioning of medical organizations. In today’s environment, hospital units work with limited resources. In fact, the efficient distribution of these resources is an essential enabler of better healthcare outcomes that improve the patients’ well-being, promote public health, and sustain the system’s development. The presented findings indicate a major degree of negative influence by the HAPUs, undermining the system’s capacity to fulfill its obligations for the community. Increased healthcare costs are an overarching theme of these discussions, meaning that HAPUs become a serious financial burden for organizations. However, in addition to this, the repercussions of unaddressed HAPUs extend beyond these ideas, contributing to the increase of mortality and readmission rates in hospitals. When all these factors act combined, the prevalence of pressure injuries translates into major healthcare issues that encompass the primary aspects of the system, in general.
In summary, there are many incidences of HAPI/HAPUs in health care settings implying that effective measures need to be taken to prevent their occurrences. They are associated with an increased hospital stay, higher cost of treatment, and they affect the overall patients’ experience. These injuries present a global healthcare concern since their magnitude tends to differ with settings. The establishment of learning points and key themes can facilitate the development of an effective solution to the problem. Since malnutrition is a major cause of high incidence rates, it is necessary to identify and implement interventions to address the issue. Efforts need to be made to identify the major root causes of HAPU to facilitate the provision of meaningful solutions (Rivera et al., 2020). Correct determination of the underlying causes can help address the social burden. This can prevent prolonged hospitalization and the involved cost due to pressure injuries.
Accumulated risk factors for the HAPU include the inability to self-ambulate, male gender, old age, extended hospital stay. Additional linen layers, hospitalized in an intensive care unit, and incontinence. Extremely low and high BMIs are linked to a high risk of developing pressure injuries (Rivera et al., 2020). Prior cases of hospital-acquired pressure injuries increase the chances of developing new instances. Spending much time in a sitting or prone setting is another factor that increases the risk. Turning and repositioning of patients can reduce chances of developing HAPU, particularly when accompanied by other interventions.
Healthcare organizations are also negatively affected by HAPUs in many ways since they hinder the ability to deliver quality medical services. Prolonged hospital stay increases the national economic burden and undermines the financial aspect of hospitals. It is necessary to establish effective avenues of addressing the problem and ensure that stronger interventions are put in place (Rivera et al., 2020). It is associated with many issues, including depleting finite resources, increasing cost, and influencing patient dissatisfaction.
Pressure Injury Prevention Bundle: Standard Risk Interventions
Pressure ulcer prevention presents a complex process since there are diverse items that need to be considered and completed. Establishing best practices is a challenging task necessitating the adoption of a care bundle to support the incorporation of the best practices. It entails the development of the best practices as well as systematically applying them. Specific care practices are beneficial in supporting the achievement of the desired outcomes. The bundle needs to incorporate various critical components, including comprehensive skin assessment, care planning, standardized risk assessment, would care nurse consult, and medical device-related interventions (Rivera et al., 2020). Standard risk interventions should consider different aspects of care and improve the existing practices. It can be tailored to a specific setting and supported with additional steps to ensure successful implementation. Key practices need to be achieved regularly to overcome the challenge of improving care. It ensures that every component of the bundle is performed consistently through the creation of a clinical pathway.
Sub-themes
Skin assessment
Comprehensive skin assessment involves the examination of the entire skin of an individual for abnormalities. It entails touching and looking at the skin while paying attention to the bony prominences. The examination is meant to detect present pressure ulcers and offer assistance in the risk stratification. This is done because patients with underlying pressure ulcers are at increased risk of developing more (Rivera et al., 2020). The assessment determines the presence of skin-related factors linked to the development of pressure ulcers, including moisture-associated skin damage (MASD) or excessively dry skin. It also enables the identification of other skin conditions and provides data required for the calculation of prevalence and incidences.
Conventionally, individuals with altered skin status are considered to have a high risk of new ulcer development. Shi (2018) argued that there lacks evidence to support the potentially prognostic relationship. The study attempted to review the existing evidence systematically to understand the relationship between the development of pressure ulcer risks and skin status. A comprehensive electronic database search was performed in February 2017 to explore longitudinal studies that used skin status to support the prediction of pressure ulcers. It considered multivariable analysis studies where two reviewers independently selected studies. Data was collected on skin status, participants, as well as the characteristics of studies. This helped gather data on multivariable analyses of pressure-ulcer and the associated skin status.
The article covered 41 studies involving 162,299 participants, out of which 7382 had new ulcers. It concluded that there exists low-certainty evidence that individuals suffering from non-blanchable erythema are at an increased risk of developing new pressure ulcers compared to those free from the condition. Low certainty evidence was noted for the prognostic effects of different ski descriptors, particularly the pressure ulcer history. This implies that there is a need for the adoption of improved preventive measures and skin assessment for patients with non-blanchable erythema.
Effective skin assessment can support early detection and influence the implementation of an appropriate intervention. Bates-Jensen Wound Assessment Tool (BWAT) can be applied in clinical practice to assess wound healing. Bates‐Jensen et al. (2019) evaluated the application of the BWAT to assess home residents with a pressure injury. The study reported pressure injury characteristics including natural history, anatomic, and stage location among racially and ethnically diverse residents. The prospective 16 weeks study covered 142 participants with 305 pressure injuries representing a prevalence of 34%. Subepidermal moisture and visual assessment were attained from heel, ischial, buttock, and sacrum ulcers every week. The study revealed that BWAT is an effective assessment tool because it offers objective and reliable data to support the detection of the progress of pressure injury healing.
Early detection and identification of pressure damage risk need to be prioritized. Kim et al. (2018) evaluated the association between the application of sub epidermal moisture measurement and visual assessment of early pressure ulceration. The study employed a descriptive prospective observational design where data was obtained from at-risk patients in Ireland within an acute care facility. Obtained data included researcher-led sub-epidermal moisture measurements and the patient’s skin condition. With a sample of 47 patients who had a mean age of 74.7 years, 19 patients suffered stage 1 pressure ulcers and elevated sub-epidermal moisture (SEM) levels. Results showed 83% specificity, where the majority of false positives lacked adequate follow-up time. The study noted a medium correlation between SEM findings and nurses’ visual skin assessment.
The SEM measurement tool required 1.5 days to detect damage, while nurses took an average of 5.5 days. This implies that SEM measurement can detect early damage about days ahead of the nurse assessment. Early detection of the pressure ulcers damage is beneficial because it develops within the deeper tissues. This can enable the adoption of effective prevention strategies before worsening the condition. Moreover, early detection can limit the associated mortality and morbidity, reduce the length of hospital stay and improve patients’ experience.
Pediatric pressure ulcers present a challenging problem in the healthcare services since it affects patients in many ways. Early detection is important to enable the establishment of effective corrective actions before the condition advances. The predictive power of Braden Q scale is controversial though it has been widely applied in the assessment of pediatric pressure ulcers. Liao et al. (2018) conducted a meta-analysis study to evaluate the scale’s predictive power for pressure ulcers among hospitalized children. Diverse databases were consulted, including CNKI, CINAHL, Cochrane Library, VIP, SinoMed, and Wangfang. Predictive value and demographic data were extracted. A MetaDiSc 1.4 was applied to calculate the pooled specificity, sensitivity as well as receiver operating characteristics (ROC). The study concluded that the Braden Q scale has a low specificity for pressure ulcers, medium sensitivity, and moderate predictive validity. This implies that the modification and development of the tool can promote the early detection of pressure ulcers among the pediatric population.
Medical Device Related Interventions
Preventing pressure ulcers (PU) is better than treating them when they develop. Turning patients is one of the interventions that is widely applied to relieve pressure from prone areas. However, medical device-related interventions exist, and they can be applied to avoid bed sores. They can benefit nursing home residents, and hospital patients can take advantage of these prevention products, such as pressure-relieving mattresses, special cushions, and heel-elevating boots. Kamikawa et al. (2018) explained that a special pressure-relieving mattress could be used to hinder the development of ulcers among patients with a high risk. Long-term facilities and hospitals should consider installing these mattresses when handling immobile, comatose as well as elderly residents and patients. They operate by lessening pressure created on the skin and enhancing the patient’s comfort. They alternate periodically to move pressure points to lower extensive pressure on one body part. They can apply a mechanical system, including deflating or inflating air cells in the mattress to attain the required comfort. Moreover, special pads can be applied to soften the surface or lower pressure and avoid the development of ulcers.
PUs are major problems affecting the health system across the globe. Yafi et al. (2017) presented preliminary case studies showing the feasibility of spatial frequency domain imaging (SFDI) to promote assessing skin status in pre-existing wounds and high-risk populations. The technology involves the use of wide-field non-contact optical imaging with structured light that is capable of examining tissue constituents and optical properties. A near-infrared SFDI system was used to image patients at an increased risk for pressure ulcers. The study concluded that SFDI is a feasible optical technology that can be applied to assess blood volume status and tissue oxygen saturation quantitatively. It can offer an effective approach for pressure ulcer healing, risk stratification, and staging.
Most of the PIs present major health issues of concern around the globe that are preventable. However, effective guidelines, equipment, commitment, and education can help identify causes, examine issues as well as offer a solution to the problem. Gupta et al. (2019) used multidisciplinary clinical and risk assessment teams to test various changes as well as implementing an effective program. The study implemented skin inspection, the surface, nutrition, incontinence, and keep moving bundle. It used PI incidence calendars, turning clocks, and signs as reminders in the unit. Addressing device-related pressure injuries was achieved by paying attention to the endotracheal tube.
Attained changed were then determined using the Plan-Do-Study-Act approach. The study revealed an 83.5% reduction in HAPI incidences and a 9.7% drop in prevalence. It was concluded that the pressure injury prevention bundle is an effective tool for the reduction of pressure injuries. This made it clear that the adoption of proper measures can help boost prevention and enable health organizations to reduce their cost of operation. The initiative presents a positive outcome to all the involved stakeholders, including patients, facility, and staff. Organizations realized cost reduction and achieve better utilization of staff resources due to fewer extended hospital stays. The reduction of the risk of PIs benefits patients since it promotes the quality of life and reduces the time spent in the hospital. Staff also benefits by achieving better job satisfaction and reduced workload. Nurses feel more satisfied with their work when they note progress among their patients. They also acquire beneficial quality improvement skills that can be applied to influence the success of other improvement projects.
Wound Care Nurse Consult
A wound care nurse consult is a healthcare professional who is experienced in wound care. The nurse is responsible for the evaluation of the effectiveness of the wound care program and offers advice to support the achievement of patients’ expectations. Working as a wound care center consultant requires one to attain the minimum educational requirements of a bachelor’s degree, several years of experience, and attain professional certification (Kazemi et al., 2018). These nurses must possess all the necessary skills, including effective communication and desire to offer quality services to patients. The ability to coordinate with other professionals, administrators, and staff is paramount in achieving the nursing objectives.
Patients with pressure ulcers depend on wound care nurses to support their treatment and avoid infections. They are involved in various critical services, including identification of the cause of wounds, development of treatment plans, mitigating infections, and caring for pressure injuries (Kazemi et al., 2018). They promote healing and show determination in the reduction of patient’s pain. They are expected to keep on improving their skills from time to time to remain relevant. This means that they need to enroll in specialized clinical training and continuing education courses. Wound care nurses consult are involved in the identification and implementation of the best care practices to hinder the development of pressure ulcers. They encourage the establishment of effective interventions to prevent the development of wounds among patients in post-acute and long-term care environments.
Education of healthcare providers, caregivers, families, and patients is important for the achievement of a proactive program of appropriate prevention interventions. Wound management requires the establishment of a comprehensive care plan to ensure that all the contributing factors are addressed. Since it is difficult to achieve a single solution to the issue, implementing a pressure injury prevention bundle is necessary to support the provision of the best care to patients (Green et al., 2018). The best outcome can be achieved by the involvement of well-educated and dedicated personnel from diverse disciplines who are working together to achieve holistic patient care. A pressure ulcer is a significant problem because it is a major cause of high mortality and morbidity. They result in increased incidences long term care compromising the quality of healthcare and patient experience.
Hospital-acquired injuries are associated with poor quality of care in a facility and can affect its reputation (Green et al., 2018). These injuries can also influence lawsuits against staff and a health care facility. This implies that managing pressure ulcers is a challenging problem that requires the adoption of a holistic approach that considers diverse aspects. Wounds affect the patient care since it is associated with many issues, including regulatory, psychosocial, emotional, financial, as well as, medical-legal aspects. Téot et al. (2020) noted that improved knowledge of the pathophysiology of wounds could help address the complex factors. The article explained the evolving and current knowledge linked to pressure ulcers while considering the effective usage of negative pressure wound therapy. Green et al. (2018) explained that consultation is beneficial in disclosing issues affecting patients that are likely to cause pressure ulcers. Patients with chronic venous leg ulcers need quality care to manage their wounds and prevent deterioration of their condition.
Gaspar et al. (2019) explained that safe patient-handling techniques could lower the risk of pressure ulcers that occurs due to shearing and friction. Prophylactic application of materials such as soft silicone sacral dressing can limit the risk of sacral pressure injuries. Wound care nurse consults recommend continuing the preventive interventions and initiating the prevention bundle to improve the quality of care to patients in a critical care setting. They also recommend the assessment of education needs before the implementation of the bundle care to establish the baseline knowledge. Offering education can improve the ability of nurses to detect the presence of pressure ulcers and understand interventions measures to limit their development. Increased awareness needs to be emphasized on key areas, including pressure ulcer prevention, development, and specific details of the prevention bundle.
Dressings that are capable of maintaining a moist wound environment are beneficial because they promote healing and can also be applied for autolytic debridement. Synthetic dressing cause less discomfort, reduce caregiver time, and offer consistent moisture. Dressing includes hydrogels, transparent films, hydrocolloids, and foams. Transparent films are effective can be used alone or in combination with hydrocolloids or hydrogels. Foams and alginates can be applied for wounds with heavy exudate because they are highly absorbent. Wound nurse care consult recommends the use of wet-to-dry dressings for debridement while avoiding them for use as a substitute. Physicians need to be familiar with the available wound dressing options to offer the best care to patients.
Summary of Standard Interventions
Patients in critical care units are at a greater risk of acquiring HAPIs. Since addressing the problem requires integrated interventions, it is important to implement a PIP bundle to standardize strategies and lower incidences of PIs. An evidence-based PIP bundle initiative involving leadership support and staff involvement has proven effective in the reduction of HAPIs and subsequent improvement of patient experience, reduction in the cost of treatment, and length of hospital. Care bundles incorporate many interventions to hinder complications and enhance preventive measures. Bundle components include skin and pressure ulcers, use of pressure-relieving devices and surfaces, risk assessment, and regular repositioning. The institute of healthcare developed the concept to enhance the consistent application of preventive measures to eliminate and reduce the risk of certain complications. Facilities can implement the approach to lower the possibility of developing pressure ulcers and promote patients’ safety.
The existing gap is that there exist limited published research studies on HAPUs, making it difficult to access sufficient information. The literature recommends health providers improve risk assessment, avoidance of shear forces and friction, and pressure redistribution as important measures for the prevention of the HAPU initiative. Risk assessment covers a comprehensive skin assessment ranging from visual inspection to physical examination. It is necessary to adopt an effective skin assessment tool to ensure consistency in the delivery of healthcare to patients.
Medical device-related interventions encourage the provision of equipment to hinder the development of pressure injuries in hospitals. Pressure redistribution surfaces such as pressure-relieving mattresses act by reducing pressure on a particular part of the body by supporting extended spreading. However, hospitals need to inspect their mattresses regularly to eliminate those that are damaged or worn out since they would achieve the desired objective.
Pressure Injury Prevention Bundle: High-Risk Interventions
Pressure injuries present major economic and clinical issues extending a detrimental impact to the health care system and patients. Most of these are hospital-acquired, implying that they are preventable through the taking of the necessary precaution. Although there is growing evidence supporting the prevention of pressure injury, there exists a gap in the implementation of effective preventative strategies. This means that pressure injuries continue causing detrimental impacts in hospitals. The pressure injury prevention care bundle is an effective approach to protect at-risk patients. This theme will provide information on high-risk interventions and explore three subthemes, namely the application of preventive dressing, turning, reposition and offloading, and other interventions.
Sub-themes
Application of Preventive dressings
Implementation of PU preventive strategies can play a role in the reduction of injury occurrences in long-term and acute settings. These injuries result in a massive economic and social burden and considerable mortality and morbidity. These sub-themes will consult various published recommendations for the application of preventive dressing in the treatment of open wounds to hinder the development of PUs. Encompassing the best practices with preventive dressing can influence the achievement of the best outcome. The application of the care bundle offers standardized methods for preventing the development of PUs.
Hahnel et al. (2020) argued that the application of dressings with the integration of the standard prevention is an effective approach in the prevention of Pus at the sacrum and heels. It involved a controlled, randomized, two-arm, superiority pragmatic study where the heels and sacrum of the intervention group were dressed. The study screened 7575 patients for eligibility, where 475 were allocated and included. The control group had 210, while the intervention group was allocated, 212 patients. The study revealed that incidences of PU among high-risk patients remain high in ICU. It made it clear that dressing of heels and sacrum, when done with additional standard preventive measures, lower absolute and relative risks for PU development. This provided evidence that preventive dressing at the sacrum and heels is a feasible approach in the prevention of PUs.
The application of preventive dressing on intact skin can significantly reduce shear forces and tension between the support surfaces and the skin. This helps lower shear forces within the underlying soft tissues and the skin. Hahnel et al. (2020) investigated whether the preventive dressing is effective when handling patients in the high-risk intensive care units. The study evaluated the effectiveness of preventive multilayered soft silicone foam dressing when applied with standard prevention approaches. The objective was to determine whether it could lower deep tissue injury (DTI) and cumulative PU incidence for categories II, III, and IV. Eligible patients were aged at least 18 years who were expected to remain in the ICU for more than 3 days. The risk assessment was based on the care dependency and mobility of patients. The study concluded that the use of preventive dressing and standard care could help prevent PUs among high-risk patients in the ICU. Unlike other interventions such as repositioning, special support surfaces, mobilization, and floating heels, the application of preventive dressing presents an easy-to-apply approach.
The use of prophylactic dressings can offer an effective strategy to support the prevention of pressure ulcers by enhancing the distribution of external pressure. They prevent friction and shear damage by hindering pressure in high-risk patients. Cornish (2017) confirmed that the application of a prophylactic dressing presents many benefits when considered in the holistic pressure ulcer prevention strategy. The dressing is examined from time to time without causing trauma or pain to patients making it an effective option. However, the article recommends nurses consider promoting hygiene and good nursing care to achieve the best outcome. The additional components of temperature, humidity, friction, and shear should motivate clinicians to establish a holistic approach to support high-risk patients. Prophylactic dressings can retain sufficient moisture to promote elasticity in the skin while reducing skin stripping, excoriation, and maceration. It also can retain the heat necessary for the healing process.
El Genedy et al. (2020) considered the cost of applying a preventive dressing and noted that they are less cost-effective and more expensive when applied on heels due to low incidences. They can generate better outcomes when applied with other PU prevention strategies. The dressing should only be applied to patients at high risk because of the economic efficiency. The analysis was conducted in a hospital setting where 422 ICU patients were analyzed. The calculated cost was based on the total for both change and application labor and applied preventive dressing. The actual number of dressings on sacrum and heels were computed, and the figure was multiplied by the unit price. The time needed for change of dressings and application was multiplied by the labor costs and then by the hourly pay for the nurses. The study recommends the involvement of all parties in both social and financial terms to determine whether to apply the approach.
Avsar et al. (2021) argued that preventive dressing could help reduce frictional forces extended to the skin since the outer surface consist of a friction resistance material. It can redistribute and absorb shear forces since they have high adhesion to the skin. The study also noted that the lateral and high loft movement is important characteristics of preventive dressing in lowering shear forces. The padding and high loft/thickness propriety reduce pressure on the body tissues enabling cushioning of bony prominences. Another important characteristic is the reduction of humidity at the dressing and skin interface. This is because the dressing allows moisture to evaporate since it is absorbent. This implies that dressing can play a role in the reduction of PU incidences and improvement of patient’s safety in ICU.
- Turning, Repositioning and Offloading (Literature review added to this theme)
- Nutrition services
Nutrition services offer patients with counseling and education on the appropriate diet based on their health condition. It focuses on well-being and overall health, and it can sometimes be considered as part of the treatment process. They are provided by a registered nutritionist or dietitian who is specialized in the area of interest. Registered dietitians apply evidence-based practice and offer reliable information based on the expected outcome. Pérez‐Escamilla & Engmann (2019) argued that PIs could be linked to malnutrition and undernutrition, explaining the importance of involving a specialist to enhance their prevention. The risk of developing PIs tends to increase when patients in critical care units become undernourished and lose weight. The dietician can guide a patient on the most appropriate diet to reduce the risk of developing PIs. Moreover, the specialist can offer guidance to support those who have already developed PIs to realize faster recovery. Billah et al. (2017) explained that increased energy and protein intake play a role in the reduction in the improvement of the healing process. Guidelines for nutritional treatment and assessment entail conducting a nutritional screening for patients at a heightened risk of developing pressure ulcers and a comprehensive nutritional assessment for those at the risk of malnutrition. It also encourages the development of a customized care plan for an individual with PIs and are malnourished. Dieticians determine the quality of food and evaluate whether they are meeting the minimum requirements by estimating the patients’ needs in terms of protein and calories.
Consultant dietitians are skilled in the identification of the causes of undernutrition, including dentition issues, dysphagia, dentition issues, loss of appetite, and other issues. They use their knowledge to offer recommendations to support the best interventions. They also coordinate with other practitioners to achieve the best nutritional needs (Billah et al., 2017). These specialists apply diverse approaches depending on issues affecting the patient and the type of wound, characteristics, and severity. This facilitates the development of the most appropriate care plan for the patient. These specialists take part in the treatment of wounds as well as in the establishment of preventive measures. They offer education and recommendations that help reduce the risk of developing PUs and improve the patient’s experience. They are also involved in goal setting, counseling, and monitoring of nutritional needs to support patients, particularly those in the critical care units.
The risk of developing PUs is high among overweight and underweight patients who are not eating a balanced diet. Maintaining a healthy weight can limit the risk of developing PUs because the skin required an adequate supply of nutrients and fluid to ensure its circulation as well as keep it supple. Underweight patients have reduced padding on bony areas increasing chances of developing PUs on areas such as hips and bottom. Having excess weight increases the weight-bearing load while reducing mobility. This exposes them to a greater risk of developing PUs because of the created excessive pressure.
Nutrition is important for the healing of PUs once they have occurred and prevent their advancement. The body requires energy, proteins, minerals, and vitamin to function properly and attain faster healing. Dietitians ensure that patients take plenty of fluid to boost their healing process. Patients with PUs are advised to take more protein since it forms the building blocks necessary for their recovery. These foods include eggs, fish, meat, beans, nuts, milk, and pulses (Pérez‐Escamilla & Engmann, 2019). It is important to ensure that patients in critical care units have at least one source of protein in all their meals. Iron is also important for the healing process, and patients are encouraged to ensure that they attain the right intake. The mineral is necessary for the maintenance of sufficient blood hemoglobin levels. They should eat such as eggs, fish, meat, beans, green vegetables, and dried fruits to ensure the right intake of iron. The food of patients in the critical care units must contain sufficient vitamin C since it promotes the absorption of iron from the food. This promotes the healing process and improves the quality of care to patients. It is necessary to ensure that their meals contain sufficient sources of vitamin C, including vegetables and fruits (Pérez‐Escamilla & Engmann, 2019). Zinc is another important mineral for patients since it plays a role in the development of new tissues.
- Other interventions in addition to high-risk interventions (Literature review added)
- Add bundle related studies at the end
- Summarize this theme
Turning, Repositioning, and Offloading
The following subtheme refers to the idea that various turning, repositioning, and offloading techniques and approaches to this intervention can lead to better patient outcomes. Repositioning and turning effectiveness is supposed to increase when medical professionals follow specific strategies to make decisions and take action. That is why the articles of this subtheme try to address appropriate research questions as to how it is possible to maximize repositioning effectiveness.
Various positioning and turning types form an area of interest for modern scholars. The study by Krapfl et al. (2017) is a literature review that has searched three databases, including CINAHL, EMBASE, and PubMed, to identify relevant articles. As a result, the scientists have extracted five research pieces that focused on the effect of incremental positioning. The findings demonstrate that this approach leads to certain changes regarding gravitational equilibrium, but this fact does not result in a reduced number of pressure injuries.
Oomens et al. (2016) selected 14 volunteers and analyzed magnetic resonance imaging (MRI) of their sacral areas. It was necessary to determine how tilting would affect individuals’ skin. The participants in a supine position demonstrate the highest strains in the muscle and fat. That is why the scholars insist that a tilting angle between 20º and 30º is optimal since it protects individuals from pressure injuries in their sacral areas.
Next, the development of effective, evidence-based turning schedules is an important component of reducing the incidence rate and impact of HAPUs. Sving et al. (2016) conduct a quasi-experimental, pre-and post-test study of 506 patients. The scientists implemented different turning schedules and assessed their impact on participants’ health. The analyzed findings demonstrate that turning schedules are not effective when used in isolation. This information indicates that it is necessary to use repositioning and turning together with additional interventions to ensure that the HAPU incidence is addressed.
A laboratory study by Wiggermann, Zhou, and McGann (2021) assesses the effectiveness of three repositioning aids, including turn and position glide sheets, pair of friction-reducing sheets, and air-assisted transfer devices, for three participants. This research demonstrates that these aids are typically insufficient to mitigate the risk of traumas. Consequently, it is not rational to rely on the interventions above to protect individuals from pressure injuries.
The findings of the current subtheme support the overall tendency that has been identified throughout the theme exploration. It relates to the fact that there is controversial evidence regarding the effectiveness of repositioning and turning in preventing pressure ulcers. These four studies have demonstrated that the same is true for various repositioning techniques and approaches. Even though the findings are controversial, it is possible to extract one typical issue. Many articles demonstrate that managing pressure injuries is a complex task that requires a comprehensive approach.
Each of the presented articles implies some limitations that deserve attention. Relatively small sample size is a limitation for some articles (Avsar et al., 2020; Mäki-Turja-Rostedt et al., 2019; Lin et al., 2020; Jocelyn Chew et al., 2018; Mussa et al., 2018; Eren, DeLuca, & Kirshblum, 2020; Krapfl et al., 2017; Oomens et al., 2017; Sharp et al., 2019; Wiggermann et al., 2021). The reliance on relatively outdated sources is a limitation of a different group of articles (Atkinson & Cullum, 2018; Latimer et al., 2017; Courvoisier et al., 2018; Pechlivanoglou et al., 2018; Lovegrove et al., 2020; Aljezawi & Tubaishat, 2018; Chitambira & Evans, 2018; Gray & Giuliano, 2018; Sving et al., 2016). The study by Gaspar et al. (2019) is limited since it does not imply coding to ensure an unbiased review of the articles. The studies’ strengths refer to the fact that the findings are consistent and reliable.
Since the articles above represent a single theme, it is not a surprise that they focus on similar variables. All of them focus on what effects turning, and repositioning can produce. The research pieces under analysis have provided some controversial findings. For example, Atkinson and Cullum (2018) and Latimer et al. (2017) admit the effectiveness of turning and repositioning, while Gaspar et al. (2019) and Mäki-Turja-Rostedt et al. (2019) state that their effect is limited. The same is found with repositioning intervals because Courvoisier et al. (2018) highlight the effectiveness of 2- and 3-hourly repositioning, while Jocelyn Chew et al. (2018) do not admit any statistically significant difference between them. This information reveals that it is reasonable to conduct a quantitative study to fill the gap regarding the effectiveness of 2-hourly repositioning. The following theme will comment on the use of turning and repositioning with other interventions to assess whether this approach is more effective.
Using Positional Pillows for Offloading
This subtheme considers whether specific pillows are sufficient to reduce pressure on individuals’ skin and protect them from pressure ulcers. Six studies are analyzed, including the works by Jiang et al. (2020), Powers (2016), Sauvage et al. (2017), Alshahrani, Sim, and Middleton (2021), Bai, Liu, Chou, and Hsu (2020), and Bambi, Yusuf, and Irwan (2020). These pieces of research try to answer research questions of whether mattresses and pillows increase turning and repositioning effectiveness in reducing the pressure ulcer incidence and mattresses of what type are better.
Jiang et al. (2020) have conducted a multicenter, open-label, and comparative study with 1,204 participants. This fact has allowed the researchers to compare the effectiveness of viscoelastic foam and air pressure redistribution mattresses. The researchers mention that the viscoelastic foam and air pressure redistribution mattresses are effective pressure injury prevention methods, but there is no significant difference between the two. According to the authors, further research is necessary to assess the mattresses’ effect for different repositioning intervals.
Powers (2016) has selected 59 participants and investigated whether the standard of care (SOC) using pillows is better than a patient positioning system (PPS) in a nonrandomized study. The scholar states that the use of pillows is not sufficient to reduce the pressure injury prevalence. It is reasonable to conduct a randomized study to investigate the given issue and identify what additional measures are necessary to solve the problem.
Simultaneously, a literature review by Bambi et al. (2020) deals with randomized controlled trials and prospective cohort studies. The scholars analyze four studies that fit their inclusion criteria. They insist that the use of 30º repositioning cushions reduces interface pressure, which, in turn, leads to a reduced incidence of pressure ulcers in healthcare facilities. It is possible to claim that these results are reliable and credible since the authors deal with a high level of evidence.
The article by Sauvage et al. (2017) is a randomized, controlled, superiority, parallel-group, open-label, multicenter study of 76 patients. The scientists have compared the effectiveness of alternating pressure air mattresses (APAM) and viscoelastic foam mattresses (VFM). The authors admit that the APAMs are more effective compared to the VFMs. It is reasonable to involve a larger sample size to test the reliability of these results and consider their generalizability.
Alshahrani et al. (2021) offer a systematic review of randomized controlled trials, quasi-experimental designs, case series, and cross-sectional studies. Analysis of 14 articles demonstrates positive outcomes of using specific surface support in addition to repositioning. This information allows for concluding that there is a robust connection between the reduced HAPU incidence and a multifaceted intervention. However, the authors assess the level of evidence as moderate or low, meaning that further research is necessary.
An observational prospective cohort study by Bai et al. (2020) compares the effectiveness of non-pressure redistributing foam mattresses and pressure redistributing ones. The sample size of 254 participants was divided into experimental and control groups with 127 members in each. The authors indicate that the use of pressure redistributing mattresses leads to a significantly reduced risk of pressure injury occurrence. These findings allow for concluding that the combination of this intervention with repositioning can lead to better outcomes.
The results of this subtheme are of significance for the major theme and overall project. The articles demonstrate that pillows, as well as viscoelastic foam and air pressure redistribution mattresses, can cope with the task. In addition to that, the subtheme indicates that APAMs are better at decreasing the incidence of pressure ulcers among older patients. It means that the research field agrees that regular repositioning can be more effective if patients use specific mattresses that reduce pressure on individuals’ skin and muscles.
Other interventions in addition to high-risk interventions
According to the information above, it is natural to discuss the use of High-risk interventions with other interventions to combat pressure injuries. This topic is requested in the research field as scholars continue to assess various additional measures’ effectiveness. The possible interventions include continuous bedside pressure mapping systems and electronic devices. Seventeen articles represent the given theme and are subdivided into appropriate subthemes.
The Use of Continuous Bedside Pressure Mapping (CBPM) Systems
The first subtheme addresses the issue that repositioning charges nurses with responsibility. It relates to the fact that many individuals forget to move to avoid pressure injuries because of various reasons. That is why it is nurses’ task to either remind them of the necessity or to reposition the patients by themselves. In this case, medical professionals need assistance to cope with the assignment successfully, and CBPM systems can be helpful in this case. These systems help nurses determine when patients start experiencing excessive pressure and when it is necessary to reposition them.
The work by Gunningberg, Sedin, Andersson, and Pingel (2017) is a pragmatic randomized controlled trial of 190 patients, including control and intervention groups. CBPM systems were applied to the intervention group to test whether the given intervention has the potential to protect older patients from pressure injuries. The authors conclude that the application of the CBPM systems does not lead to any significant improvement regarding pressure injury incidence. It means that further research is necessary to test whether the blinded intervention will have the same impact on patient health.
Simultaneously, Gunningberg and Carli (2016) have conducted a prospective and quantitative study of 19 registered nurses and 33 assistant nurses, where the medical professionals assessed the effectiveness of CBPM. This approach allows the researchers to find that healthcare professionals highly appraise the instrument, stating that this intervention leads to optimized repositioning, which is helpful to reduce pressure ulcers. Further research is necessary to investigate the patients’ perception of CBPM systems.
Hultin et al. (2019) offer a qualitative, descriptive study of 31 orthopedic patients who are 65 years old and higher. They participated in semi-structured interviews, and their answers were subject to qualitative content analysis. This approach allows for identifying that the CBPM system increases adults’ awareness of pressure injuries and the necessity to prevent them. It denotes that this instrument is significant for patients to make them more engaged in HAPU prevention measures.
The given subtheme demonstrates that both medical professionals and patients positively assess the use of CBPM to prevent pressure injuries. This instrument implies some benefits because regular notifications of the necessity to change the patients’ position are convenient for all the stakeholders. Qualitative methodologies produce these results, while a randomized controlled trial by Gunningberg et al. (2017) does not identify reduced HAPU incidence. Further research implying a blind intervention is necessary to find the actual effect of CBPM systems. These findings reveal that this topic is considered using different methodologies, meaning that the given DPI project is not interested in addressing this topic.
Additional Electronic Devices
This subtheme refers to the issue that appropriate electronic devices can improve the effect of repositioning and turning to reduce pressure injury incidence. This topic is addressed by a few relevant and timely studies that represent different methodologies. The studies try to answer the research question of whether various electronic devices, including automatic repositioning systems, wearable patient sensors, accelerometers, and others, can decrease the incidence of pressure injuries.
Edger (2017) conducts a prospective before-and-after study with 717 patients to test a repositioning device’s impact. The author also focuses on the cost-effectiveness of the given intervention. This repositioning device reduces the pressure injury incidence from 1.3% to 0%, while the return on investment accounts for more than $16,000 (Edger, 2017, p. 236). This information reveals that the tool under analysis maximizes the repositioning and turning advantages.
Knibbe, Zwaenepoel, Knibbe, and Beeckman (2018) assess the effect of an automatic repositioning system on 13 patients over four weeks to analyze how an automated repositioning system can influence their skin. The authors admit that an automatic repositioning system leads to recovery from pressure ulcers. This article is another research piece that supports the idea that the combination of turning and repositioning with additional technological tools is beneficial for patients.
Minteer et al. (2019) analyze two sensor devices that imply no contact with the patient skin to track ten individuals’ movements. The scholars organize a specific experiment to assess this tool’s effectiveness. The study reveals that the sensor devices accurately track patient movements. This finding allows for concluding that medical professionals can rely on these devices to monitor if patients engage in regular repositioning and address this situation if some inefficiencies exist.
The study by Pickham et al. (2019) is a randomized clinical trial that includes 1,312 participants divided into control and experimental groups to evaluate the use of a wearable patient sensor. The experiment demonstrates that the tool under analysis is helpful since it makes patients change their positions every two hours. This approach results in the fact that the article offers arguments to support the effectiveness of 2-hourly repositioning.
Richardson, Peart, Wright, and McCullagh. (2017) conduct a quality improvement program that took place in four adult critical care units with 88 beds in total to test the use of technical and non-technical interventions. The study reveals that wearable sensors lead to lower pressure ulcer rates. In particular, the authors claim that the HAPU incidence reduced by 63% over four years (Richardson et al., 2017, p. 433). Consequently, it is rational to rely on devices to address HAPUs.
Duvall, Karg, Brienza, and Pealrman (2019) assess the effectiveness of the E-scale monitoring system for preventing pressure injuries among ten participants. The study reveals that the tool under analysis is capable of identifying patient movements with an increased level of accuracy. It denotes that the E-scale system can be considered a helpful instrument for healthcare professionals to monitor bed movements and promote them among patients when required.
A study by Yap, Kennerly, and Ly (2019) follows a mixed-method, pre-and post-test design. The scholars focus on 44 residents and 38 staff participants to identify whether a patient monitoring system can increase repositioning compliance. The study results demonstrate that this approach can increase the effectiveness of 2-hourly repositioning among nursing home residents. Consequently, this electronic device implies essential advantages that make it a helpful tool in preventing HAPUs.
Stinson, Ferguson, and Porter-Armstrong (2018) analyze the findings of two recent articles with at-risk cohorts, including 21 participants in total. The study assesses the use and impact of accelerometers and interface pressure mapping systems. It is the only study that fails to highlight the positive effects of using electronic devices. The scholars admit that accelerometers and interface pressure mapping systems are not effective in preventing pressure injuries.
The studies of this subtheme demonstrate that the use of electronic devices can improve the effectiveness of repositioning in combating pressure ulcers. Even though some research pieces may not identify positive outcomes, most articles reveal that medical professionals and establishments should make an effort to choose the most suitable interventions. These findings show a consistent set of literature that proves the effectiveness of using electronic devices to manage HAPUs.
The articles from this theme have certain limitations that deserve attention. Firstly, some studies are limited because they focus on small sample sizes (Hultin et al., 2019; Sauvage et al., 2017; Powers, 2016; Alshahrani et al., 2021; Bambi et al., 2020; Knible et al., 2018; Minteer et al., 2018; Stinson et al., 2018; Duvall et al., 2019; Yap et al., 2019). Secondly, other studies are narrow-focused, meaning that their results cannot be generalized (Gunningberg & Carli, 2016; Gunningberg et al., 2017; Jiang et al., 2020; Bai et al., 2020; Edger, 2017; Pickham et al., 2019; Richardson et al., 2017). That is why the scholars make specific efforts to ensure that these limitations are addressed. Some of them rely on reputable review guidelines (Alshahrani et al., 2021; Bambi et al., 2020), while others invest in following scientific principles to increase the level of evidence.
These results support the findings of Theme 1 that turning and repositioning are effective when used with additional interventions. It denotes that there is no gap in this area, meaning that the scientific processes of the DPI project should focus on turning and repositioning in isolation. Quantitative articles from Theme 2 demonstrate that this methodology can provide the required information to identify the effectiveness of quality improvement initiatives. The following section will determine how it is possible to affect HAPUs.
Summary of literature review
Patients in ICU are usually inactive, exposing them to the risk of developing HAPIs. The use of the PIP bundle can support the standardization of PIP strategies and influence a reduction in pressure ulcers. An evidence-based PIP bundle initiative needs support from the leadership and involved staff. The impact on the patient outcome negatively and hinders nurse satisfaction. They are associated with the increased cost of medication, prolonged hospital stay, poor patient experience, and a high rate of mortality. Risk factors for HAPIs development include sedation, immobility, hemodynamic instability, and vasopressors.
The management of PIP is an interdisciplinary approach, and its basic components include debriding necrotic tissue, relieving and reducing pressure on the skin, managing bacterial colonization and load, and identifying wound dressing. Pressure-reducing devices have proven effective in the prevention of HAPI in critical care settings. Static devices are appropriate when supporting patients who can independently change positions. An air-fluidized or low-air-loss bed is effective for patients with non-healing or multiple large ulcers. It is necessary to evaluate pain during debridement, dressing changes, and repositioning. Pain needs to be eliminated by adjusting pressure-reduction surfaces, covering the wound, and systematic analgesia.
The reduction of HAPIs and the implementation of PIP bundle necessitates a comprehensive approach while establishing a sense of ownership among nurses, involvement, engagement, and support of every stakeholder. The PIP bundle initiative is enhanced when health care workers show commitment to the provision of quality care to patients. Reducing HAPIs as well as maintaining the momentum is a major challenge affecting many critical care units. Implementing the integrated approach is an expensive process making it difficult for many hospitals to adopt despite its benefits. Moreover, there exists a gap in the literature, and further research is needed to improve the level of bundle evidence for the PIP implementation.
Limitations in the implementation of the PIP bundle care is the existence of environmental and patient variables that are likely to interfere with HAPI rates during the implementation process. This would affect the validity of the intervention because of the other influencing factors. Another limitation is that the PIP bundle required follow-up to ensure its sustainability. This calls for more commitment from nurses and facility administrators. Since the approach requires the integration of diverse care approaches, it requires the involvement of different disciplines and strong coordination. It necessitates improvement of communication to ensure that all the involved staff works together towards the achievement of desired objectives.
The project is important to be conducted because it encourages critical care units to implement PIP bundles to prevent patients from developing pressure ulcers. It is necessary to prevent the development of PUs because they are associated with poor functional recovery, and they increase chances of infections and pain, as well as extending the hospital stay. They can contribute to high mortality rates and are an indication of a poor overall prognosis. The project can enable health practitioners and critical care facilities to achieve their objectives of offering quality care to patients. PUs increases pressure on patients and compromises their ability to respond to treatment. This implies that health organizations should not hesitate to implement PIP to promote patients’ experience and reduce their stay in the hospital. The design of the project is applicable in diverse settings enabling its implementations in different facilities. Health providers should consider investing in the PIP bundle to boost their service to patients.
Data Analysis and Results
The purpose of this chapter is to summarize the collected data, how it was analyzed and then to present the results. This section of Chapter 4 briefly restates the problem statement, the methodology, the clinical question(s) or phenomena, and then offers a statement about what will be covered in this chapter. Chapter 4 should present the results of the project as clearly as possible, leaving the interpretation of the results for Chapter 5. Make sure this chapter is written in past tense and reflects how the project was actually conducted.
This chapter typically contains the analyzed data, often presented in both text and tabular or figure format. To ensure readability and clarity of findings, structure is of the utmost importance in this chapter. Sufficient guidance in the narrative should be provided to highlight the findings of greatest importance for the reader. Most investigators begin with a description of the sample and the relevant demographic characteristics presented in text or tabular format.
Ask the following general questions before starting this chapter:
- Is there sufficient data to answer each of the clinical question(s) asked in the project? (see Appendix C) One procedure for determining a sample size ahead of the project is a power analysis.
- Is there sufficient data to support the conclusions you will make in Chapter 5? (see Appendix D) If using SPSS version 26 to perform analyses, the data is entered and coded using numbers or numerical codes.
- Is the project written in the third person? Never use the first person.
- Is the data clearly explained using a table, graph, chart, or text? (see Appendix E)
Visual organizers, including tables and figures, must always be introduced, presented and discussed within the text first. Never insert them without these three steps. It is often best to develop all of the tables, graphs, charts, etc. before writing any text to further clarify how to proceed. Point out the salient results and present those results by table, graph, chart, or other form of collected data. See Appendix E for examples of APA formatted tables and figures.
Descriptive Data
This section of Chapter 4 provides a narrative summary of the population or sample characteristics and demographics of the participants in the project. It establishes the number of subjects, gender, age, education level or employee classification, (if appropriate), organization, or setting (if appropriate), and other appropriate sample characteristics (e.g. education level, program of project, employee classification etc.). The use of graphic organizers, such as tables, charts, histograms and graphs to provide further clarification and promote readability, is encouraged to organize and present coded data. Ensure this data cannot lead to anyone identifying individual participants in this section or identifying the data for individual participants in the data summary and data analysis that follows.
For numbers, equations, and statistics, spell out any number that begins a sentence, title, or heading – or reword the sentence to place the number later in the narrative. In general, use Arabic numerals (10, 11, 12) when referring to whole numbers 10 and above, and spell out whole numbers below 10. There are some exceptions to this rule:
If small numbers are grouped with large numbers in a comparison, use numerals (e.g., 7, 8, 10, and 13 trials); but, do not do this when numbers are used for different purposes (e.g., 10 items on each of four surveys).
- Numbers in a measurement with units (e.g., 6 cm, 5-mg dose, 2%).
- Numbers that represent time, dates, ages, sample or population size, scores, or exact sums of money.
- Numbers that represent a specific item in a numbered series (e.g., Table 1).
A sample table in APA style is presented in Table 3. Be mindful that all tables fit within the required margins, and are clean, easy to read, and formatted properly using the guidelines found in Chapter 5 (Displaying Results) of the APA Publication Manual 7th Edition.
Table 3: A Sample Data Table Showing Correct Formatting
Note. Adapted from “Sampling and Recruitment in Studies of Doctoral Students,” by I.M. Investigator, 2010, Journal of Perspicuity, 25, p 100. Reprinted with permission.
Data Analysis Procedures
This section presents a description of the process that was used to analyze the data. If clinical question(s) guided the project, data analysis procedures can be framed relative to each clinical question. Data can also be organized by chronology of phenomena, by themes and patterns, or by other approaches as deemed appropriate according for the project. The key components included in this section are:
- A detailed description of the data analysis procedures.
- An explanation of how the raw data relates to the clinical questions(s) asked in the project for a quantitative project.
- A discussion of the identification of sources of error and their effect on the data.
- An explanation and justification of any differences in why the data analysis section does not match what was approved in Chapter 3 (if appropriate).
- An analysis of the reliability and validity of the data in statistical terms, for quantitative projects.
Results
This section, which is the primary section of this chapter, presents a summary and analysis of the data in a non-evaluative, unbiased, organized manner that relates to the clinical question(s). List the clinical question(s) as you are discussing them in order to ensure that the readers see that the question has been addressed. Answer the clinical question(s) in the order that they are listed for quantitative studies. The key components included in this section are:
- The data and the analysis of that data should be presented in a narrative, non-evaluative, unbiased, organized manner by clinical question(s).
- The section should also include appropriate graphic organizers, such as tables, charts, graphs, and figures.
- The amount and quality of the data or information is sufficient to answer the clinical question(s) is well presented, and is intelligently interpreted.
- Quantitative: Findings are presented by clinical question using section titles. They are presented in order of significance, if appropriate.
- Quantitative: Results of each statistical test are presented in appropriate statistical format with tables, graphs, and charts.
- Quantitative: For inferential statistics, p-value and test statistics are reported.
- Quantitative: Control variables (if part of the design) are reported and discussed. Outliers, if found, were reported.
The results must be presented without implication, speculation, assessment, evaluation, or interpretation. Discussion of results and conclusions are left for Chapter 5. Refer to the APA Style Manual for additional lists and examples. In quantitative practice improvement projects, it is not required for all data analyzed to be presented; however, it is important to provide descriptive statistics and the results of the applicable statistic tests used in conducting the analysis of the data. It is also important that there are descriptive statistics provided on all variables. Nevertheless, it is also acceptable to put most of this in the Appendix if the chapter becomes too lengthy.
Required components include descriptive and inferential statistics. Descriptive statistics describe or summarize data sets using frequency distributions (e.g., to describe the distribution for the IQ scores in your class of 30 pupils) or graphical displays such as bar graphs (e.g., to display increases in a school district’s budget each year for the past five years), as well as histograms (e.g., to show spending per child in school and display mean, median, modes, and frequencies), line graphs (e.g., to display peak scores for the classroom group), and scatter plots (e.g., to display the relationship between two variables). Descriptive statistics also include numerical indexes such as averages, percentile ranks, measures of central tendency, correlations, measures of variability and standard deviation, and measures of relative standing.
Inferential statistics describe the numerical characteristics of data, and then go beyond the data to make inferences about the population based on the sample data. Inferential statistics also estimate the characteristics of populations about population parameters using sampling distributions, or estimation. Table 4 presents example results of an independent t test comparing Emotional Intelligence (EI) mean scores by gender.
Table 4: t-Test for Equality of Emotional Intelligence Mean Scores by Gender
After completing the first draft of Chapter 4, ask these general questions:
- Are the findings clearly presented, so any reader could understand them?
- Are all the tables, graphics or visual displays well-organized and easy to read?
- Are the important data described in the text?
- Is factual data information separate from analysis and evaluation?
- Are the data organized by clinical questions?
Chapter 4 can be challenging with regard to mathematical equations and statistical symbols or variables. When including an equation in the narrative, space the equation as you would words in a sentence: x + 5 = a. Punctuate equations that are in the paragraph, as you would a sentence. Remember to italicize statistical and mathematical variables, except Greek letters, and if the equation is long or complicated, set it off on its own line.
Refer to your APA manual for specific details on representation of statistical information. Basic guidelines include:
- Statistical symbols are italicized (t, F, N, n)
- Greek letters, abbreviations that are not variables and subscripts that function as identifiers use standard typeface, no bolding or italicization
- Use parentheses to enclose statistical values (p =.026) and degrees of freedom t(36) = 3.85 or F(2, 52) = 3.85
- Use brackets to enclose limits of confidence intervals 95% CIs [- 5.25, 4.95]
Make sure to include appropriate graphics to present the results. Always introduce, present, and discuss the visual organizers in narrative form. Never insert a visual organizer without these three steps.
A figure is a graph, chart, map, drawing, or photograph. Below is an example of a figure labeled per APA style. Do not include a figure unless it adds substantively to the understanding of the results or it duplicates other elements in the narrative. If a figure is used, a label must be placed under the figure. As with tables, refer to the figure by number in the narrative preceding the placement of the figure. Make sure a table or figure is not split between pages. Below is another example of a table and figure for you to review. (see Table 5 and Figure 4)
Table 5: The Servant Leader
Note. Derived from Laub, J. (1999). Assessing the servant organization: Development of the servant organizational leadership assessment (SOLA) instrument (Doctoral Practice improvement project). Available from ProQuest Practice improvement project and Theses Database. (UMI No. 9921922)
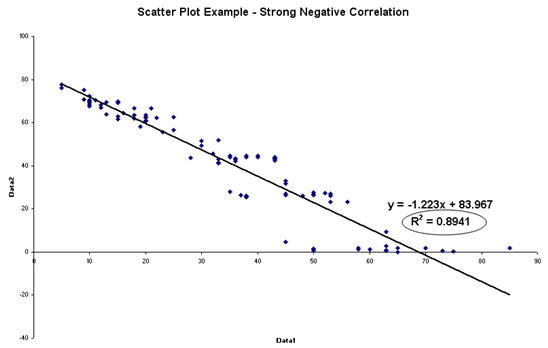
Note, An example of a strong negative correlation for SAT composite score and time spent on Facebook for 11th grade high school students enrolled in IMSmart SAT Prep Course.
Summary
This section provides a concise summary of what was found in the project. It briefly restates essential data and data analysis presented in this chapter, and it helps the reader see and understand the relevance of the data and analysis to the clinical question(s). Finally, it provides a lead or transition into Chapter 5, where the implications of the data and data analysis relative to the clinical question(s) will be discussed. The summary of the data must be logically and clearly presented, with the factual information separated from interpretation. For quantitative studies, summarize the statistical data and results of statistical tests in relation to the clinical question(s). Finally, provide a concluding section and transition to Chapter 5.
Summary, Conclusions, and Recommendations
This section introduces Chapter 5 as a comprehensive summary of the entire project. It reminds the reader of the importance of the topic and briefly explains how the project intended to contribute to the body of knowledge on the topic. It informs the reader that conclusions, implications, and recommendations will be presented.
Chapter 5 is perhaps the most important chapter in the practice improvement project manuscript because it presents the investigator’s contribution to the body of knowledge. For many who read evidence-based literature, this may be the only chapter they will read. Chapter 5 typically begins with a brief summary of the essential points made in Chapters 1 and 3 of the original DPI project and includes why this topic is important and how this project was designed to contribute to the understanding of the topic. The remainder of the chapter contains a summary of the overall project, a summary of the findings and conclusions, recommendations for future practice, and a final section on implications derived from the project.
No new data or citations should be introduced in Chapter 5; however, references should be made to findings or citations presented in earlier chapters. The investigator can articulate new frameworks and new insights. The concluding words of Chapter 5 should emphasize both the most important points of the project and what the reader should take from them. This should be presented in the simplest possible form, making sure to preserve the conditional nature of the insights. Refer to the University practice improvement project rubric for guidance on the content of this chapter.
Summary of the Project
This section provides a comprehensive summary of the overall project that describes the content of the project to the reader in the simplest possible terms. It should recap the essential points of Chapters 1-3, but it should remain a broad, comprehensive view of the project. It reminds the reader of the clinical question(s) and the main issues being evaluated, and provides a transition, explains what will be covered in the chapter and reminds the reader of how the project was conducted.
Summary of Findings and Conclusion
This section of Chapter 5 is organized by clinical question(s), and it conveys the specific findings of the project. The section presents conclusions made based on the data analysis and findings of the project and relates the findings back to the literature, significance of the project in Chapter 1, advancing scientific knowledge in Chapter 1. Significant themes/ findings are compared and contrasted, evaluated and discussed in light of the existing body of knowledge. The significance of every finding is analyzed and related to the significance section and advancing scientific knowledge section of Chapter 1. Additionally, the significance of the findings is analyzed and related back to Chapter 2, and ties the project together. The findings are bounded by the DPI project parameters described in Chapters 1 and 3, are supported by the data and theory, and directly relate to the clinical question(s). No unrelated or speculative information is presented in this section. This section of Chapter 5 should be organized by clinical question(s), theme, or any manner that allows summarizing the specific findings supported by the data and the literature. Conclusions represent the contribution to knowledge and fill in the gap in the knowledge. They should also relate directly to the significance of the project. The conclusions are major generalizations, and an answer to the practice problem developed in Chapters 1 and 2. This is where the project binds together. In this section, personal opinion is permitted, as long as it is backed with the data, grounded in the project methods and supported in the literature.
Implications
This section should describe what could happen because of this project. It also tells the reader what the DPI project results imply theoretically, practically, and for the future. Additionally, it provides a retrospective examination of the theoretical framework presented in Chapter 2 in light of the practice improvement project’s findings. A critical evaluation of the strengths and weaknesses of the project, and the degree to which the conclusions are credible given the methodology, project design, and data, should also be presented. The section delineates applications of new insights derived from the practice improvement project to solve real and significant problems. Implications can be grouped into those related to theory or generalization, those related to practice, and those related to future projects. Separate sections with corresponding headings provide proper organization.
Theoretical Implications
Theoretical implications involve interpretation of the practice improvement project findings in terms of the clinical question(s) that guided the project. It is appropriate to evaluate the strengths and weaknesses of the project critically and include the degree to which the conclusions are credible given the method and data. It should also include a critical, retrospective examination of the framework presented in the Chapter 2 Literature Review section in light of the practice improvement project’s new findings.
Practical Implications
Practical implications should delineate applications of new insights derived from the practice improvement project to solve real and significant problems.
Future Implications
Two kinds of implications for future projects are possible: one based on what the project did find or do, and the other based on what the project did not find or do. Generally, future DPI projects could look at different kinds of subjects in different kinds of settings, interventions with new kinds of algorithms or dependent measures, or new theoretical issues that emerge from the project. Recommendations should be included on which of these possibilities are likely to be most fruitful and why.
Recommendations
Summarize the recommendations that result from the project. Each recommendation should trace directly to a conclusion.
Recommendations for Future Projects
This section should contain a minimum of four to six recommendations for future DPI projects, as well as a full explanation for why each recommendation is being made. Additionally, this section discusses the areas of project that need further examination, or addresses gaps or new patient or system needs the project found. The section ends with a discussion of “next steps” in forwarding this line of DPI project evaluations. Recommendations relate back to the project significance and advancing scientific knowledge sections in Chapter 1.
Recommendations for Practice
This section should contain two to five recommendations for future practice based on the results and findings of the project, as well as a full explanation for why each recommendation is being made. It provides a discussion of who will benefit from reading and implementing the results of the project and presents ideas based on the results that practitioners can implement in the work or educational setting. Unrelated or speculative information that is unsupported by data is clearly identified as such. Recommendations should relate back to the project significance section in Chapter 1.
Appendix C
Power Analysis Using G Power
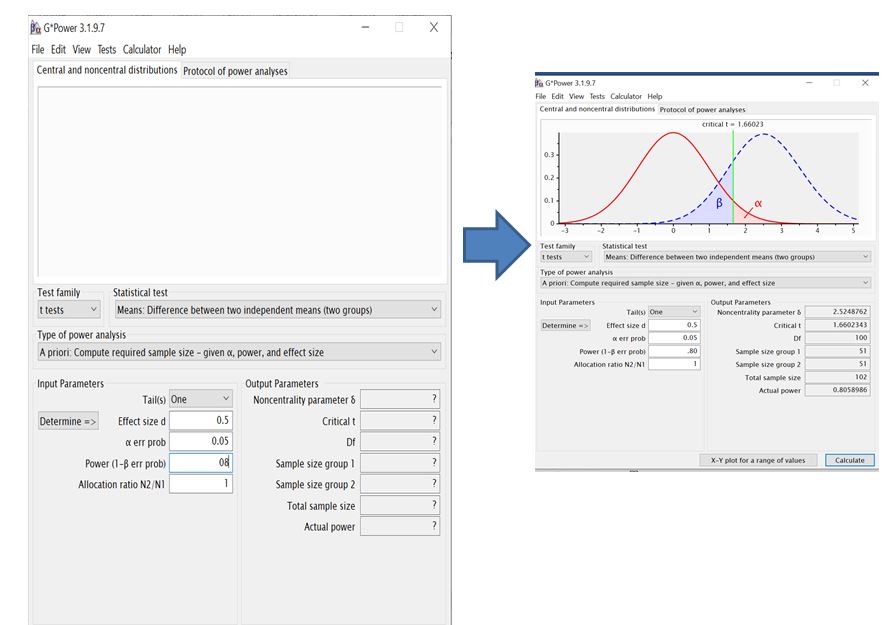
Appendix D
Example SPSS Dataset & Variable View
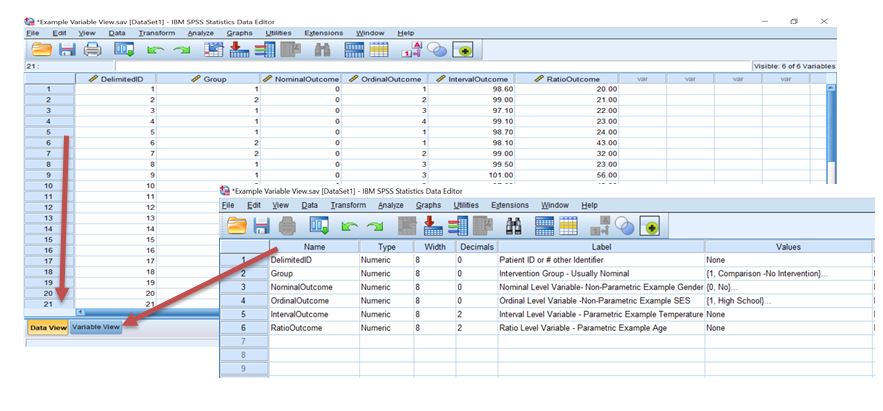
The SPSS database is set up with all variables coded to compare between or within the comparison groups. A comparison may be made within the same individual and it coded 1 for before and 2 after the intervention. Or if measuring between individuals, the data would be coded the same 1 for before and 2 after as noted in the Group Column. Software supplied by University.
Appendix E
How to Make APA Format Tables and Figures Using Microsoft Word
Tables vs. Figures
- See APA Publication Manual, Chapter 7 for additional details (APA, 2019).
- Tables consist of words and numbers where spatial relationships usually do not indicate any numerical information.
- Tables should be used to present information that would be too wordy, repetitive, or difficult to read as text.
- Figures typically communicate numerical information using spatial relations. For example, as you move up the Y axis of bar graph the scores usually go up.
Examples of APA Tables
Descriptive table
Table 1: Characteristics of Variables
Note. Add notes here = (Provide any reference, 2019).
Table 2:Number of Handoff Per Groups
Note. SBAR handoff was defined as …. (IHI, 2020)
Table 3: Number of Hours Per Week Spent in Various Activities
Note. Schoolwork was defined as time spent doing class work outside of regular class time.
*statistically significant at p <.05
Chi-Square example (Group IV x Group DV)
Table 1:Crosstabulation of Gender and Chronic Pain
Note. Adjusted standardized residuals appear in parentheses below group frequencies
**= p <.01.
t-Test Example (Dichotomous Group IV x Score DV)
Notice two separate t-test results have been reported.
Table 1: Chronic Paint Score and Exercise time for Males and Females
Note. Standard Deviations appear in parentheses below means.
* = p <.05, *** = p <.001.
One Way ANOVA with 3 Groups Example (Group IV x Score DV)
Remember with an ANOVA, you have to report paired comparisons associated with post hoc or planned comparisons) for significant analyses. The results of paired comparisons are indicated by the subscripts on the means within rows. Also, notice in this table that we report the results of four separate analyses. This is the real power of tables: we can convey a large amount of information very concisely.
Table 1: Analysis of Variance for Sleep Times and Experimental Groups
Standard deviations appear in parentheses bellow means. Means with differing subscripts within rows are significantly different at the p <.05 based on Fisher’s LSD post hoc paired comparisons.
* = p <.05, *** = p <.001.
Factorial ANOVA Example 2 x 3 between subject’s design
Notice that two tables are used here. The first table reports the overall results for the 2×3 factorial ANOVA, which includes the Main Effects for the two IV’s and the Interaction Effect for the two IV’s. The second table reports the means and simple effects tests for the significant interaction effect.
Table 1: Experimental Group x Sex Factorial Analysis of Variance for Sleep Scores
Table 2: Analysis of Sleep Scores for Experimental Groups by Gender
Note. Standard deviations appear in parentheses bellow means. Means with differing subscripts within rows are significantly different at the p <.05 based on Fisher’s LSD post hoc paired comparisons.
** = p <.01
Notice that the simple effect comparing the 3 experiment groups only for females, requires follow up tests in order to determine which groups are significantly different. In this case, Fisher’s LSD test was used, and the results are represented with the different subscripts for each mean. In this case, female participants in the Aerobic exercise group did not differ from the no exercise group so they are given the same subscript (a). However, women in the control group and women in the Weight lifting group significantly differed from the Aerobic watching group and so the Weight Lifting group was labeled with a different subscript (b). The male subjects did not differ from one another, so they all share the same subscript (a).
Correlations (Scores IV x Scores IV)
Table 1: Pearson’s Product Moment Correlations for Chronic Pain Score, Exercise Attitude Scores and Physical Activity
† = p < .10, *= p < .05, **= p < .01, ***= p < .001.
Examples of APA Figures
Generally, the same features apply to figures as have been previously provided for tables: They should be easy to read and interpret, consistent throughout the document when presenting the same type of figure, kept on one page if possible, and supplement the accompanying text or table.
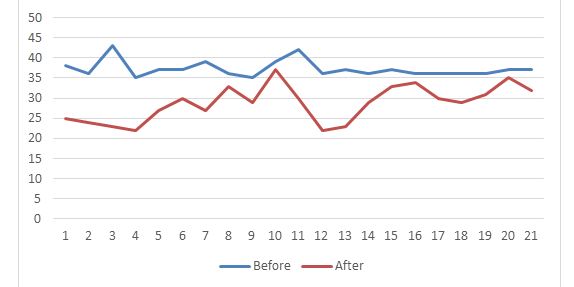
Note: Reprinted from S. GCU. Or Adapted from or www.website.com. Reprinted with permission.
If the figure is not your own work, note the source or reference where you found the figure. Write, “Reprinted from” or “Adapted from,” followed by the title of the book, article, or website where you found the figure. Include the page number where you found the figure as well if you are citing a figure from a book. If you are citing a figure from a website, you may write, “Reprinted from The Huffington Post.” Or include the author’s first and second initial as well as their surname. Use the author’s first and second initial, if available, rather than the author’s full first name. Note their last name as well.
References
American Psychological Association [APA]. (2019). Publication manual of the American Psychological Association. (7th ed.). Washington, DC; Author Microsoft Word ®. (2019).
Bates‐Jensen, B. M., McCreath, H. E., Harputlu, D., & Patlan, A. (2019). Reliability of the Bates‐Jensen wound assessment tool for pressure injury assessment: The pressure ulcer detection study. Wound Repair and Regeneration, 27(4), 386-395. Web.
Gaspar, S., Peralta, M., Marques, A., Budri, A., & Gaspar de Matos, M. (2019). Effectiveness on hospital‐acquired pressure ulcers prevention: a systematic review. International Wound Journal, 16(5), 1087-1102. Web.
Green, J., Jester, R., McKinley, R., & Pooler, A. (2018). Chronic venous leg ulcer care: Putting the patient at the heart of leg ulcer care. Part 1: exploring the consultation. British Journal of Community Nursing, 23(Sup3), S30-S38. Web.
Green, J., Jester, R., McKinley, R., & Pooler, A. (2018). Chronic venous leg ulcer care: Putting the patient at the heart of leg ulcer care. Part 1: exploring the consultation. British Journal of Community Nursing, 23(Sup3), S30-S38. Web.
Gupta, P., Shiju, S., Chacko, G., Thomas, M., Abas, A., Savarimuthu, I., Omari, E., Al-Balushi, S., Jessymo, P., Mathew, S., Quinto, M., McDonald, I., & Andrews, W. (2020). A quality improvement programme to reduce hospital-acquired pressure injuries. BMJ Open Quality, 9(3), e000905. Web.
Kamikawa, N., Hamada, H., Sekikawa, K., Yamamoto, H., Fujika, Y., Kajiwara, T.,… & Otoyama, I. (2018). Posture and firmness changes in a pressure-relieving air mattress affect cough strength in elderly people with dysphagia. PloS one, 13(12), e0208895. Web.
Kazemi, A., Carnaggio, K., Clark, M., Shephard, C., & Okoye, G. A. (2018). Optimal wound care management in hidradenitis suppurativa. Journal of Dermatological Treatment, 29(2), 165-167. Web.
Kazemi, A., Carnaggio, K., Clark, M., Shephard, C., & Okoye, G. A. (2018). Optimal wound care management in hidradenitis suppurativa. Journal of Dermatological Treatment, 29(2), 165-167. Web.
Kim, C. G., Park, S., Ko, J. W., & Jo, S. (2018). The relationship of subepidermal moisture and early stage pressure injury by visual skin assessment. Journal of Tissue Viability, 27(3), 130-134. Web.
Liao, Y., Gao, G., & Mo, L. (2018). Predictive accuracy of the Braden Q Scale in risk assessment for paediatric pressure ulcer: A meta-analysis. International journal of nursing sciences, 5(4), 419-426. Web.
Rivera, J., Donohoe, E., Deady-Rooney, M., Douglas, M., & Samaniego, N. (2020). Implementing a Pressure Injury Prevention Bundle to Decrease Hospital-Acquired Pressure Injuries in an Adult Critical Care Unit: An Evidence-Based, Pilot Initiative. Wound Management & Prevention, 66(10), 20-28.
Shi, C., Dumville, J. C., & Cullum, N. (2018). Skin status for predicting pressure ulcer development: a systematic review and meta-analyses. International Journal of Nursing Studies, 87, 14-25. Web.
Téot, L., Geri, C., Lano, J., Cabrol, M., Linet, C., & Mercier, G. (2020). Complex wound healing outcomes for outpatients receiving care via telemedicine, home health, or wound clinic: a randomized controlled trial. The International Journal of Lower Extremity Wounds, 19(2), 197-204. Web.
Téot, L., Geri, C., Lano, J., Cabrol, M., Linet, C., & Mercier, G. (2020). Complex wound healing outcomes for outpatients receiving care via telemedicine, home health, or wound clinic: a randomized controlled trial. The International Journal of Lower Extremity Wounds, 19(2), 197-204. Web.
Yafi, A., Muakkassa, F. K., Pasupneti, T., Fulton, J., Cuccia, D. J., Mazhar, A.,… & Mostow, E. N. (2017). Quantitative skin assessment using spatial frequency domain imaging (SFDI) in patients with or at high risk for pressure ulcers. Lasers in Surgery and Medicine, 49(9), 827-834. Web.
Billah, S. M., Saha, K. K., Khan, A. N. S., Chowdhury, A. H., Garnett, S. P., Arifeen, S. E., & Menon, P. (2017). Quality of nutrition services in primary health care facilities: Implications for integrating nutrition into the health system in Bangladesh. PloS one, 12(5), e0178121. Web.
Pérez‐Escamilla, R., & Engmann, C. (2019). Integrating nutrition services into health care systems platforms: Where are we and where do we go from here. Maternal & child nutrition, 15, e12743. Web.
Appendix F
Writing up your statistical results
Identify the analysis technique: In the results section (Chapter 4), your goal is to report the results of the data analyses used to answer your project question. To do this, you need to identify your data analysis technique, report your test statistic, and provide some interpretation of the results. Each analysis you run should be related to your clinical question or PICOT. If you analyze data that is exploratory or outside your clinical question, you need to indicate this in the results.
Format test statistics: Test statistics and p values should be rounded to two decimal places (If you are providing precise p-values for future use in meta-analyses, 3 decimal places is acceptable). All statistical symbols (sample statistics) that are not Greek letters should be italicized (M, SD, t, p, etc.).
Indicate the direction of the significant difference: When reporting a significant difference between two conditions, indicate the direction of this difference, i.e. which condition was more/less/higher/lower than the other condition(s). Assume that your audience has a professional knowledge of statistics. Do not explain how or why you used a certain test unless it is unusual (i.e., such as a non-parametric test).
How to report p values: Report the exact p value (this is the preferred option if you want to make your data convenient for individuals conducting a meta-analysis on the topic).
Example: t(33) = 2.10, p =.03.
If your exact p value is less than.001, it is conventional to state merely p <.001. If you report exact p values, state early in the results section the alpha level used as a significance criterion for your tests. For example: “We used an alpha level of.05 for all statistical tests.”
If your results are in the predicted direction but are not significant, you can say your results were marginally significant. Example: Results indicated a marginally significant preference for pie (M = 3.45, SD = 1.11) over cake (M = 3.00, SD =.80), t(5) = 1.25, p =.08.
If your p-value is over.10, you can say your results revealed a non-significant trend in the predicted direction. Example: Results indicated a non-significant trending in the predicted direction indicating a preference for pie (M = 4.25, SD = 2.21) over cake (M = 3.25, SD = 2.60), t(5) = 1.75, p =.26.
Descriptive Statistics
Mean and Standard Deviation are most clearly presented in parentheses:
- The sample as a whole was relatively young (M = 19.22, SD = 3.45).
- The average age of students was 19.22 years (SD = 3.45).
Percentages are also most clearly displayed in parentheses with no decimal places:
- Nearly half (49%) of the sample was married.
Frequencies or rates are reported including the range, mode, or median.
T-tests
There are several different designs that utilize a t-test for the statistical inference testing. The differences between one-sample t-tests, related measures t-tests, and independent samples t tests are clear to the knowledgeable reader so eliminate any elaboration of which type of t-test has been used. Additionally, the descriptive statistics provided will identify which variation was employed. It is important to note that we assume that all p values represent two-tailed tests unless otherwise noted and that independent samples t-tests use the pooled variance approach (based on an equal variances assumption) unless otherwise noted:
- There was a significant effect for gender, t(54) = 5.43, p <.001, with men receiving higher scores than women.
- Results indicate a significant preference for pie (M = 3.45, SD = 1.11) over cake (M = 3.00, SD =.80), t(15) = 4.00, p =.001.
- The 36 study participants had a mean age of 27.4 (SD = 12.6) were significantly older than the university norm of 21.2 years, t(35) = 2.95, p =.01.
- Students taking statistics courses in psychology at the University of Washington reported studying more hours for tests (M = 121, SD = 14.2) than did UW college students in general, t(33) = 2.10, p =.034.
- The 25 participants had an average difference from pre-test to post-test anxiety scores of -4.8 (SD = 5.5), indicating the anxiety treatment resulted in a significant decrease in anxiety levels, t(24) = -4.36, p =.005 (one-tailed).
- The 36 participants in the treatment group (M = 14.8, SD = 2.0) and the 25 participants in the control group (M = 16.6, SD = 2.5), demonstrated a significance difference in performance (t[59] = -3.12, p =.01); as expected, the visual priming treatment inhibited performance on the phoneme recognition task.
- UW students taking statistics courses in Psychology had higher IQ scores (M = 121, SD = 14.2) than did those taking statistics courses in Statistics (M = 117, SD = 10.3), t(44) = 1.23, p =.09.
- Over a two-day period, participants drank significantly fewer drinks in the experimental group (M= 0.667, SD = 1.15) than did those in the wait-list control group (M= 8.00, SD= 2.00), t(4) = -5.51, p=.005.
ANOVA and post hoc tests
ANOVAs are reported like the t test, but there are two degrees-of-freedom numbers to report. First report the between-groups degrees of freedom, then report the within-groups degrees of freedom (separated by a comma). After that report the F statistic (rounded off to two decimal places) and the significance level.
One-way ANOVA:
- The 12 participants in the high dosage group had an average reaction time of 12.3 seconds (SD = 4.1); the 9 participants in the moderate dosage group had an average reaction time of 7.4 seconds (SD = 2.3), and the 8 participants in the control group had a mean of 6.6 (SD = 3.1). The effect of dosage, therefore, was significant, F(2,26) = 8.76, p=.012.
- An one way analysis of variance showed that the effect of noise was significant, F(3,27) = 5.94, p =.007. Post hoc analyses using the Scheffé post hoc criterion for significance indicated that the average number of errors was significantly lower in the white noise condition (M = 12.4, SD = 2.26) than in the other two noise conditions (traffic and industrial) combined (M = 13.62, SD = 5.56), F(3, 27) = 7.77, p =.042.
- Tests of the four a priori hypotheses were conducted using Bonferroni adjusted alpha levels of.0125 per test (.05/4). Results indicated that the average number of errors was significantly lower in the silence condition (M = 8.11, SD = 4.32) than were those in both the white noise condition (M = 12.4, SD = 2.26), F(1, 27) = 8.90, p =.011 and in the industrial noise condition (M = 15.28, SD = 3.30), F (1, 27) = 10.22, p =.007. The pairwise comparison of the traffic noise condition with the silence condition was nonsignificant. The average number of errors in all noise conditions combined (M = 15.2, SD = 6.32) was significantly higher than those in the silence condition (M = 8.11, SD = 3.30), F(1, 27) = 8.66, p =.009.
Multiple Factor (Independent Variable) ANOVA:
- There was a significant main effect for treatment, F(1, 145) = 5.43, p <.01, and a significant interaction, F(2, 145) = 3.13, p <.05.
- The cell sizes, means, and standard deviations for the 3×4 factorial design are presented in Table 1. The main effect of Dosage was marginally significant (F[2,17] = 3.23, p =.067), as was the main effect of diagnosis category, F(3,17) = 2.87, p =.097. The interaction of dosage and diagnosis, however, has significant, F(6,17) = 14.2, p =.0005.
- Attitude change scores were subjected to a two-way analysis of variance having two levels of message discrepancy (small, large) and two levels of source expertise (high, low). All effects were statistically significant at the.05 significance level. The main effect of message discrepancy yielded an F ratio of F(1, 24) = 44.4, p <.001, indicating that the mean change score was significantly greater for large-discrepancy messages (M = 4.78, SD = 1.99) than for small-discrepancy messages (M = 2.17, SD = 1.25). The main effect of source expertise yielded an F ratio of F(1, 24) = 25.4, p <.01, indicating that the mean change score was significantly higher in the high-expertise message source (M = 5.49, SD = 2.25) than in the low-expertise message source (M = 0.88, SD = 1.21). The interaction effect was non-significant, F(1, 24) = 1.22, p >.05.
- A two-way analysis of variance yielded a main effect for the diner’s gender, F(1,108) = 3.93, p <.05, such that the average tip was significantly higher for men (M = 15.3%, SD = 4.44) than for women (M = 12.6%, SD = 6.18). The main effect of touch was nonsignificant, F(1, 108) = 2.24, p >.05. However, the interaction effect was significant, F(1, 108) = 5.55, p <.05, indicating that the gender effect was greater in the touch condition than in the non-touch condition.
Chi Square
Chi-Square statistics are reported with degrees of freedom and sample size in parentheses, the Pearson chi-square value (rounded to two decimal places), and the significance level:
- The percentage of participants that were married did not differ by gender, X2(1, N = 90) = 0.89, p >.05.
- The sample included 30 respondents who had never married, 54 who were married, 26 who reported being separated or divorced, and 16 who were widowed. These frequencies were significantly different, X2 (3, N = 126) = 10.1, p =.017.
- As can be seen by the frequencies cross tabulated in Table xx, there is a significant relationship between marital status and depression, X2 (3, N = 126) = 24.7, p <.001.
- The relation between these variables was significant, X2 (2, N = 170) = 14.14, p <.01. Catholic teens were less likely to show an interest in attending college than were Protestant teens.
- Preference for the three sodas was not equally distributed in the population, X2 (2, N = 55) = 4.53, p <.05.
Correlations
Correlations are reported with the degrees of freedom (which is N-2) in parentheses and the significance level: The two variables were strongly correlated, r(55) =.49, p <.01.
Regression analyses
Regression results are often best presented in a table. A PA doesn’t say much about how to report regression results in the text, but if you would like to report the regression in the text of your Results section, you should at least present the standardized slope (beta) along with the t-test and the corresponding significance level. (Degrees of freedom for the t-test is N-k-1 where k equals the number of predictor variables.) It is also customary to report the percentage of variance explained along with the corresponding F test.
Social support significantly predicted depression scores, b = -.34, t(225) = 6.53, p <.01. Social support also explained a significant proportion of variance in depression scores, R2 =.12, F(1, 225) = 42.64, p <.01.
Tables
Add a table or figure: Adding a table of figure can be helpful to the reader. See the current APA Publication manual for examples. In reporting the results of statistical tests, report the descriptive statistics, such as means and standard deviations, as well as the test statistic, degrees of freedom, obtained value of the test, and the probability of the result occurring by chance (p value).
- APA style tables do not contain any vertical lines.
- There are no periods used after the table number or title.
- When using columns with decimal numbers, make the decimal points line up.
- Use MS Word tables to create tables
American Psychological Association [APA]. (2019). Publication manual of the American Psychological Association (7th ed.). Washington, DC: Author.

