Abstract
Communication is the most fundamental component that determines the success of all care processes. Communication conceptual framework can help understand various aspects of active sharing of information and issues that lead to communication failures and strategies to overcome them. Healthcare provider-patient communication framework comprises four key components: participants’ communication goals, participants themselves, communication process, and environment in which their interaction occurs. Linear, interactional, and transactional communications models are the poplar representation of processes of communication. Caregivers and patients use different types and channels of communication to convey messages. The different types of feedback provided in communication are positive, negative, positive feedforward and negative feedforward. Barriers to effective communication in healthcare settings may be inevitable but can be minimized. Environmental factors such as noise and personal factors can hinder communication between caregivers and patients. Health care provides play the most fundamental role in promoting effective communication between them and the clients to ensure improved patient outcomes.
Introduction
Delivery of quality as safe care in healthcare institutions takes more than diagnosis and performing various procedures. Communication is the most fundamental component that determines the success of all care processes. Accurate sharing f patient information between health facilities or among the team of nurses, doctors, and specialist requires effective communication. Poor communication in health care is costly since it can contribute to critical malpractices, leading to complications and even patient deaths. Therefore, hospitals and other healthcare organizations need strong communications designed to guarantee patients’ well-being. Effective communication in the healthcare sector involves everyone in the continuum of care, ranging from managers to patients and their families. Evaluating a communication conceptual framework can help understand various aspects of active sharing of information and issues that lead to communication failures and strategies to overcome them.
Conceptual Framework for Healthcare Providers-Patient Communication
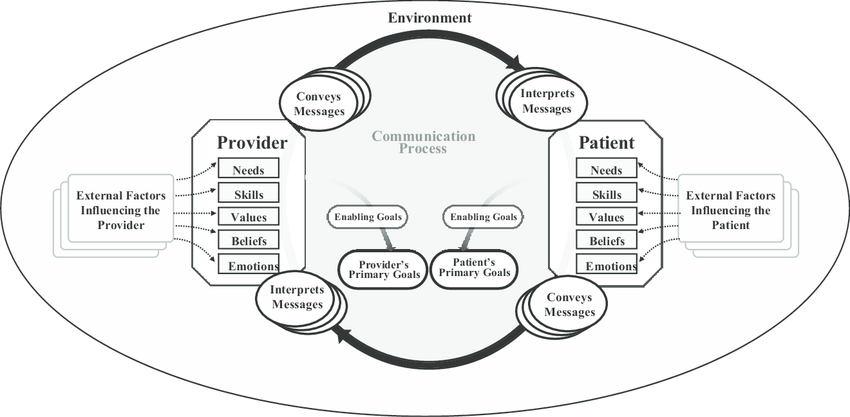
This paper presents a conceptual framework of communication between healthcare providers and patients. As noted in the introduction, communication is an important factor influencing the quality and outcome of care delivery. The framework comprises four key components: participants’ communication goals, participants themselves, communication process, and environment in which their interaction occurs. Notably, while the patients’ primary goal is to seek quality health care services, doctors’ and nurses’ main objective is to deliver the latter to ensure individual ad social well-being (Rathnayake et al., 2021). Various factors such as values, skills, beliefs, and emotions influence care providers’ and patients’ communication. The communication process involves formulating, transmitting, and interpreting messages and then giving feedback. It is important to note that the communication between the participants is a dynamic process that uses different channels. The environment refers to the settings in which the communication occurs, for example, doctors’ offices or hospital wards.
Types of Communication Models
Models of communication are instrumental in explaining the social process of creating and conveying messages. Communication is learned behavior, even if it occurs in different ways that involve the use of symbols to create and interpret meaning. The most popular models of communication are linear, interactional, and transactional. The models simplify communication’s basic structure and facilitate a better understanding of the latter. The models provide a diverse element of communication and explain the interrelation of different parts of the communication process.
Linear Communication Model
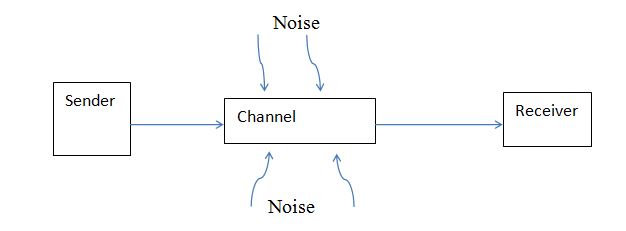
The model considers communication a linear process, where senders transmit messages to the recipients. The conveyed message may comprise behaviors, sounds, or words that allow communication interaction. A channel or route for communication is used to transmit the message to the receiver. The model acknowledges the presence of obstacles or noise that may hinder the process of communication (Pierce, 2019). A linear communication model has limitations, even if it is simple and easier to understand. Developers of this model assumed a person could only be a receiver or a sender, whereas communication is a dynamic process with recipients not being just passive. The model also provides one channel for a particular message and implies the latter has a distinct beginning and end.
Interactional Model of Communication
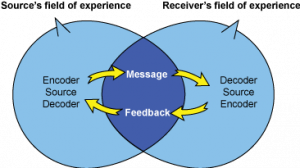
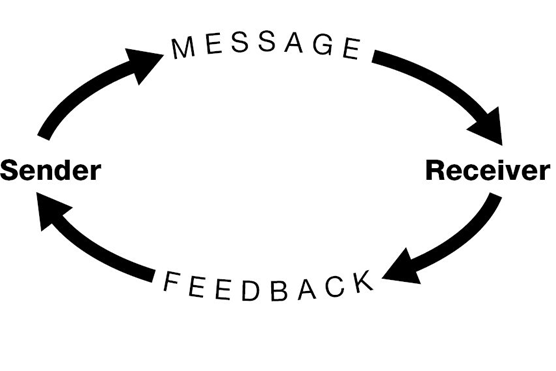
The model views communication as an ongoing process by focusing on conveyed messages and feedback. The model follows two channels in which message and feedback between senders and recipients. Notably, feedback is a verbal or non-verbal response given to the senders and receivers, indicating comprehension of the message. The field of experience feature of this model refers to various factors such as environment, culture, and experiences that can influence the construction of messages (Pierce, 2019). It is imperative to note that every communication interaction is unique since every party involved brings a distinctive field of experience. A notable limitation of the interactional communication model is that involved individuals cannot be senders and receivers simultaneously.
Transactional Model of Communication
This model is the most dynamic compared to the previous models of communication. The transactional model refers to the people as communicators without differentiating between senders and receivers. This aspect implies that individuals have to send and receive messages to achieve communication. Pierce (2019) notes that the transactional model considers communication as a cooperative action where involved parties co-create the process, effectiveness, and outcome of the interaction.
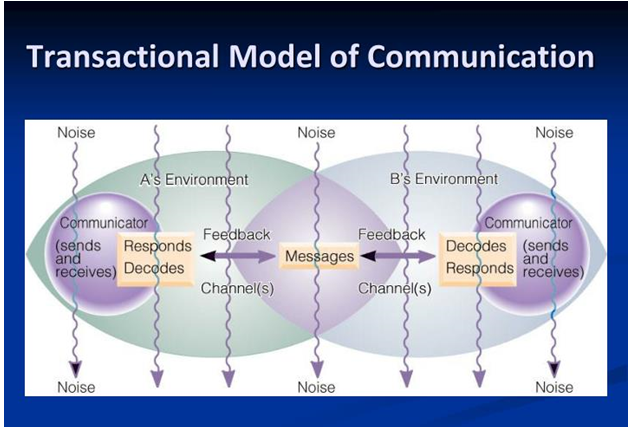
The transactional model emphasizes some shared degree of environment, language, and culture among people for them to communicate effectively. The model further acknowledges that messages influence responses produced during communication interaction. Pierce (2019) indicates that the view of people as dynamic communicators, messages as interdependent, and the necessity of overlapped fields of experience to establish a shared meaning in the transactional model make an instrumental foundation for communication theory. Therefore, this model portrays a clear picture of clear communication between individuals.
Communication Feedback Loop
A communication feedback loop refers to a process whereby one party involved in an interaction initiates and sends a message with an objective that the recipient will satisfy that goal. Senders open the loop when they initiate the communication with the idea that the receiver will close it by giving the desired feedback. The involved parties in care provider-patient communication can be senders as well as receivers. Doctors or nurses can ask patients how they are feeling (opening the feedback loop) and responds by giving experiences due to illness (closing the loop).
Types of Feedback in Communication
Feedback in communication is vital because it determines the subsequent direction of a conversation. Different types of feedback provided in communication are positive, negative, positive feedforward and negative feedforward. For instance, if a nurse-patient conversation is about a behavior influencing a particular illness, positive feedback from the care provider would affirm the client’s conduct and encourage him or her to continue doing the same. Conversely, negative feedback would be a corrective comment about past behavior in relation to the management of a particular disease. Positive feedforward feedback would be an affirmation of what should be done in the future to successfully prevent or manage a disease. Negative feedforward feedback would be about what the patient should not repeat in the future.
Types of Communication
People use verbal, non-verbal, and written communication to convey their messages. Verbal communication involves the use of worlds to exchange information or messages. Verbal communication is spontaneous and can be through face-to-face or telephone conversations. This type gives involved parties a channel to get feedback immediately after receiving messages. Individuals should know their audiences, use appropriate language and tone, speak clearly, and respond in the best way possible to guarantee effective communication. Non-verbal communication uses body language, eye contact, gestures, pitch, and appearances to send messages.
Written communication uses recorded or printed materials such as memos, requirement analysis documents, minutes of a meeting, and plans to convey meaningful messages. This type of communication provides well-thought and planned details. Although written communication can be time-consuming and response is not immediate, it can be useful for future reference. Visual communication is another type used, especially in the healthcare sector, to deliver messages and information through visual aids or graphical presentations. Visual communication complements verbal, non-verbal, and written communications, creating a more effective way of understanding messages.
Communication Channels
Communication channels refer to the various ways used by people to convey messages. Sharing information as well as asking questions and answering are fundamental in healthcare settings. For instance, healthcare providers ask patients questions to gather all information that can help in the diagnosis and treatment of diseases. Equally, physicians and nurses answer any question of concern to the patients. Notably, care provider-patient communication goes beyond within healthcare facilities. The diferent communication channels used to facilitate interaction between care providers and patients include face-to-face, phone calls, emails, text messages, and patient portals.
Face-to-face communication is the most common channel used by all people. The interesting thing today is that people do not have to be physically in the same room for them to have a face-to-face conversation. This channel of communication is important since it is necessary to grasp non-verbal messages in certain situations. Healthcare providers always use face-to-face communication to assess, treat and monitor the progress of their patients. Technologies such as telehealth also allow care providers to meet with their patients virtually. Telehealth supports care delivery by making services more convenient for patients with limited time, mobility, and transportation options. Additionally, it enhances communication and coordination between the healthcare team and patients.
Phone calls and text messages are everyday channels of communication used by most people. Phone calls are the fastest, most direct, and most effective way of conveying messages and getting responses from people in a different physical location. Alternatively, people send text messages when their intended recipients cannot be reached over the phone. Healthcare providers and patients use phone calls as their channel of communication for important or urgent conversations that do not require visual cues. For instance, physicians or nurses can call patients to remind them about the time to take medicine, adhering to prescription, and next appointment. They can also use text messages as quick and unobtrusive means of sending directly as simple messages.
Emails and patient portals are also communication channels used in various organizations. Email is the fastest and most popular written communication channel, which is ideal when one wants to keep a record of the conversation. Health care providers and patients can use this channel for reminders, appointment confirmations, and post-visit surveys. For instance, nurses can send surveys to get patients’ feedback, which engages the clients and strengthens the care providers’ reputation. A patient portal is the most convenient means by which patients can access their medical information. Patient portals also facilitate immediate response to frequently asked questions, and it generates a positive attitude from patients, helping improve the latter’s engagement and retention.
Barriers to Effective Communication between Healthcare Providers and Patients
Effective communication is fundamental in the delivery of quality care services to patients. However, various environmental and personal factors impede active interaction between patients and care providers, negatively impacting care quality and patient satisfaction. Effective communication allows care providers to as much information as possible needed to make the correct diagnosis and design an appropriate treatment plan. Therefore, it is imperative to ensure that there is no or minimal element hindering patient-care provider’s communication.
Environmental Barriers to Communication
Noise, privacy, and time constraints are some of the environmental factors that hurt effective communication between care providers and their patients. Background noises within a busy clinical setting can negatively impact patients’ ability to hear. Noise and other distractions within a clinical room can inhibit interaction with patients with cognitive disorders such as dementia (Ali, 2017). Some patients may be unwilling or uncomfortable to give sensitive personal information if they think people within their surroundings can hear it, for example, in hospital wards where curtains are used for privacy. Inadequate time causes a significant barrier to communication for care providers. Nurses are more likely to neglect the quality of communication due to competing demands for attention from the patients. Ali (2017) indicates that conversations between care providers and patients may be interrupted or delayed in pressured clinical settings because of other clients’ needs. For instance, a nurse may be required to respond to pain relief or emergency while in the middle of communication with a patient. The latter can feel neglected and become frustrated, further hindering subsequent interaction.
Personal Barriers to Communication
Values and beliefs are important personal factors that can hinder effective communication between caregivers and patients. Individuals make assumptions based on their cultural values, beliefs, and traditions. For example, some patients might believe that men cannot be midwives. Equally, nurses may assume that patients from Arabic countries cannot speak good English or persons with a learning disability are not in healthy relationships. Such assumptions are likely to share information that is vital in diagnosis, treatment, and monitoring of progress.
Symptoms such as pain and fatigue can reduce patients’ concentration, hindering effective communication (Ali, 2017). Patients in severe pain or who are distressed and acutely ill may be less attentive, making it challenging for the health care providers to collect important information from them. Some medications can cause side effects such as drowsy, sleeplessness, and fatigue (Wune et al., 2020). Therefore, patients may become less alert making it challenging for them to have a healthy conversation with caregivers.
Embarrassment and anxiety among patients can also prevent them from sharing information with doctors and nurses. Not everyone is comfortable in talking about challenging family circumstances, sex, or undressing in front of total strangers. Some patients may be worried about causing embarrassment by using inappropriate terms or about undergoing invasive medical examinations (Ali, 2017). Others may be reluctant to seek clarification or ask questions since they fear wasting the care provider’s time. Such awkward encounters between patients and nurses or doctors can significantly hinder effective communication.
Language differences and the use of jargon further make interactions between care providers and patients difficult. Doctors and nurses are likely to receive whose English is not their national language, making it challenging to gather and understand information from them. Healthcare professionals from a similar field of practice use jargon as a communication aid (Ali, 2017; Abdulla et al., 2022)). However, using clinical acronyms and technical jargon with patients can hamper communication.
Overcoming the Barriers to Effective Communication
Healthcare providers and patients can adopt various approaches to overcome different factors that can hinder their communication. Caregivers should minimize background noises or move to a quiet room if they think their clients have hearing problems (Ali, 2017). They can also request patients to complete forms to avoid asking sensitive questions in a setting where other people can hear the responses. Acknowledging the pain and discomfort the patients are experiencing and showing empathy can help establish rapport and encourage them to communicate (Ali, 2017). Giving clear directions and using open communication can minimize embarrassment and anxiety, easing difficult conversations. Healthcare professionals should also avoid using acronyms technical jargon with the patients to facilitate better understanding and appropriate feedback.
Discussion
Health care provider-patient communication is an inseparable component in every healthcare setting. Effective communication between nurses and patients is fundamental to quality care services (Amoah et al., 2019; Tran et al., 2020; Kwame & Petrucka, 2021). Effective communication facilitates the provision of healthcare services that meet and respect the needs of both caregivers and patients, promoting the perception of quality care and positive outcomes. Kwame and Petrucka (2021) propose the development and implementation of patient-centered communication in all healthcare settings indicating that it is an instrumental tool for guaranteeing optimal health outcomes. Such communication can allow individualized care services that respond to patients’ beliefs, health concerns, and contextual variables. However, patient-centered communication encounters various hindrances. The obstacles can be categorized into environmental, personal, behavioral, communication, institutional, and system-related barriers (Kwame & Petrucka, 2021). These hurdles occur in the process of communication as the involved parties try to achieve their goals, as shown in the conceptual framework.
The quality of communication caregiver-patient interaction can vary significantly depending on the involved parties. According to Tran et al. (2020), a significant number of nurses have inadequate skills that facilitate all-round communication. Only a small percentage of care providers can effectively use verbal, non-verbal, and other forms of communication to interact with the patients. Molina-Mula and Gallo-Estrada (2020) add that lack of active communication provokes tension, further inhibiting sharing of information between patients and caregivers. Kwame and Petrucka (2020) highlight poor communication skills, inadequate staffing, and excessive workload among care providers as key factors that hinder effective communication. Such findings are an indicator that much needs to be done in the healthcare sector to promote effective communication between patients and care providers.
The significance of effective care provider-patient communication necessitates appropriate actions to facilitate and promote it. Caregivers have an instrumental role in ensuring effective communication between them and the patients. Therefore, the person-centered care and communication continuum (PC4) model proposed by Kwame and Petrucka (2021) can be a milestone towards achieving patient-centered communication in healthcare. The key components of the model include task-centered communication, process-centered communication, and person-centered communication. The model can help health care providers to choose and employ appropriate forms and channels of communication, ensuring enhanced patient and caregiver experiences as well as improved positive outcomes.
Conclusion
Communication in healthcare settings is an instrumental tool that influences all aspects of care delivery. People can better understand the interaction between care providers and patients using a conceptual framework that shows key components, including participants’ communication goals, participants themselves, communication process, and environment in which their interaction occurs. Although there are different communication models, the transactional model portrays a clear picture of the interaction between patients and caregivers. The types and channels of communication in healthcare vary depending on involved parties and the goals of sending a particular message. Nevertheless, barriers to effective communication may be inevitable, requiring appropriate actions to alleviate the impacts of the hindrances. Health care provides play the most fundamental role in promoting effective communication between them and the clients to ensure improved patient outcomes.
References
Abdulla, N., Naqi, R., & Jassim, G. (2022). Barriers to nurse-patient communication in primary healthcare centers in Bahrain: Patient perspective. International Journal of Nursing Sciences, 1-23. Web.
Ali, M. (2017). Communication skills 2: Overcoming the barriers to effective communication. Nursing Times, 114(1), 40-42.
Amoah, V., Anokye, R., Boakye, D., Acheampong, E., Budu-Ainooson, A., & Okyere, E. et al. (2019). A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nursing, 18(1), 1-8. Web.
Kwame, A., & Petrucka, P. (2020). Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. International Journal of Africa Nursing Sciences, 12, 1-24. Web.
Kwame, A., & Petrucka, P. (2021). A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nursing, 20(1), 1-10. Web.
Molina-Mula, J., & Gallo-Estrada, J. (2020). Impact of Nurse-Patient Relationship on Quality of Care and Patient Autonomy in Decision-Making. International Journal Of Environmental Research And Public Health, 17(3), 1-24. Web.
Pierce, T. (2019). The evolution of human communication: From theory to practice. Ecampusontario.pressbooks.pub. Web.
Rathnayake, S., Dasanayake, D., Maithreepala, S., Ekanayake, R., & Basnayake, P. (2021). Nurses’ perspectives of taking care of patients with Coronavirus disease 2019: A phenomenological study. PLOS ONE, 16(9), 1-17. Web.
Tran, T., Tran, T., Nguyen, A., Dinh, T., Le, A., & Tran, H. et al. (2020). Nurse–patient communication: A quality assessment in public hospital. International Journal of Healthcare Management, 14(4), 1127-1133. Web.
Wune, G., Ayalew, Y., Hailu, A., & Gebretensaye, T. (2020). Nurses to patients’ communication and barriers perceived by nurses at Tikur Anbessa Specilized Hospital, Addis Ababa, Ethiopia 2018. International Journal of Africa Nursing Sciences, 12, 1-5. Web.

